A 55 Year Old Client Reports Cessation Of Menstrual Periods
Breaking News Today
Mar 15, 2025 · 6 min read
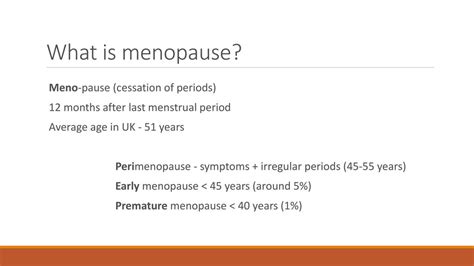
Table of Contents
Menopause: Understanding the Cessation of Menstrual Periods in a 55-Year-Old Client
Menopause, the permanent cessation of menstruation, is a natural biological process marking the end of a woman's reproductive years. For a 55-year-old client reporting this cessation, it's crucial to understand the multifaceted aspects of this transition, both physically and emotionally. This article delves into the physiological changes, diagnostic considerations, potential complications, management strategies, and the psychosocial impact of menopause on a woman at this age.
Understanding the Physiology of Menopause
Menopause is characterized by the depletion of ovarian follicles, leading to a decline in estrogen and progesterone production. This hormonal shift triggers a cascade of physiological changes throughout the body. The average age of menopause is 51, but it's perfectly normal for it to occur between 45 and 55 years of age. Our 55-year-old client falls within this expected range.
The Role of Hormones
Estrogen, the primary female sex hormone, plays a vital role in regulating the menstrual cycle, maintaining bone density, influencing cardiovascular health, and contributing to skin elasticity. Progesterone, another crucial hormone, prepares the uterus for pregnancy. As ovarian function declines, the production of both estrogen and progesterone significantly decreases, leading to the cessation of menstruation and a range of associated symptoms.
Physiological Changes Associated with Menopause
The hormonal decline during menopause doesn't just affect the reproductive system. It impacts various bodily systems, leading to a constellation of symptoms, often referred to as menopausal symptoms. These can vary widely in severity and duration from woman to woman. Common symptoms include:
- Vasomotor symptoms: Hot flashes, night sweats, and palpitations are among the most prevalent symptoms. These are caused by fluctuations in blood vessel dilation and constriction.
- Sleep disturbances: Insomnia, difficulty falling asleep, and frequent awakenings are common due to hormonal shifts and hot flashes.
- Genitourinary changes: Vaginal dryness, itching, and painful intercourse (dyspareunia) are common due to decreased estrogen levels affecting the vaginal tissues. Urinary incontinence may also occur.
- Mood changes: Irritability, anxiety, depression, and mood swings are frequently reported. These changes are often linked to hormonal fluctuations and the emotional impact of this life transition.
- Cognitive changes: Some women experience difficulties with memory, concentration, and cognitive function.
- Musculoskeletal changes: Decreased bone density (osteoporosis) and increased risk of fractures are major concerns. Muscle mass may also decrease.
- Cardiovascular changes: The risk of heart disease increases after menopause due to changes in cholesterol levels and blood vessel function.
- Skin and hair changes: Skin becomes drier and thinner, and hair may thin or become brittle.
Diagnosing Menopause
While a 55-year-old client reporting cessation of menstrual periods for 12 consecutive months strongly suggests menopause, a thorough evaluation is crucial to rule out other potential causes of amenorrhea (absence of menstruation).
Differential Diagnoses
It’s important to consider other conditions that might mimic menopause, such as:
- Premature ovarian failure (POF): This condition involves the cessation of ovarian function before the age of 40.
- Hypothyroidism: Underactive thyroid can lead to irregular or absent periods.
- Hyperprolactinemia: Elevated prolactin levels can suppress ovulation and menstruation.
- Other endocrine disorders: Conditions affecting the pituitary gland or hypothalamus can disrupt the hormonal balance that regulates menstruation.
- Stress: Significant stress can temporarily disrupt the menstrual cycle.
- Certain medications: Some medications, such as chemotherapy drugs, can induce amenorrhea.
Diagnostic Tests
Depending on the client's history and presentation, the physician might order several tests, including:
- Hormone level testing: Measuring follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estradiol levels can help confirm ovarian function. Elevated FSH and LH levels are indicative of menopause.
- Thyroid function tests: To rule out hypothyroidism.
- Prolactin level test: To check for hyperprolactinemia.
- Other tests: Depending on the clinical picture, other investigations, such as ultrasound or blood tests, may be necessary.
Management and Treatment Options
The management of menopause focuses on alleviating symptoms and mitigating long-term health risks. Treatment is individualized based on the client's specific needs and preferences.
Lifestyle Modifications
Lifestyle changes can significantly improve menopausal symptoms:
- Regular exercise: Reduces hot flashes, improves mood, and supports bone health.
- Healthy diet: A balanced diet rich in fruits, vegetables, and whole grains supports overall health.
- Stress management techniques: Yoga, meditation, and deep breathing exercises can help reduce stress and anxiety.
- Sleep hygiene: Establishing a regular sleep schedule and creating a relaxing bedtime routine can improve sleep quality.
- Weight management: Maintaining a healthy weight is crucial for cardiovascular health and bone density.
Hormone Therapy (HT)
Hormone therapy (HT), also known as hormone replacement therapy (HRT), involves supplementing estrogen and/or progesterone to alleviate menopausal symptoms. It's a highly effective treatment for vasomotor symptoms, vaginal dryness, and mood disturbances. However, the decision to use HT should be individualized, carefully considering the potential benefits and risks based on the client's age, medical history, and risk factors.
Types of HT:
- Estrogen-only therapy: Suitable for women who have had a hysterectomy (removal of the uterus).
- Combined estrogen-progesterone therapy: Used in women who still have their uterus to prevent endometrial hyperplasia (thickening of the uterine lining).
Potential Risks of HT: While HT can significantly alleviate symptoms, potential risks need careful consideration, including: increased risk of blood clots, stroke, and breast cancer. The risks and benefits should be discussed thoroughly with the healthcare provider.
Non-Hormonal Treatments
Several non-hormonal treatments are available to manage specific menopausal symptoms:
- Selective serotonin reuptake inhibitors (SSRIs): Can help manage mood disturbances and hot flashes.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): Similar to SSRIs in managing mood and hot flashes.
- Gabapentin: Can be effective in reducing hot flashes and sleep disturbances.
- Clonidine: Can alleviate hot flashes.
- Vaginal lubricants and moisturizers: Relieve vaginal dryness and dyspareunia.
- Low-dose vaginal estrogen therapy: Provides localized estrogen treatment to alleviate vaginal symptoms without systemic effects.
Psychosocial Impact and Support
Menopause is not just a physiological event; it’s a significant life transition with psychosocial implications. The cessation of menstruation can symbolize the end of reproductive capacity, triggering emotional responses such as grief, anxiety, and a sense of loss.
Emotional Well-being
Supporting the client's emotional well-being during this transition is crucial. Open communication, empathy, and providing resources are essential. Consider referring the client to a therapist or counselor specialized in perimenopause and menopause if needed.
Social Support
Social support plays a vital role in navigating menopause. Encouraging connections with family, friends, or support groups can provide emotional solace and practical advice.
Long-term Health Implications
Managing menopause effectively is crucial for long-term health. Addressing issues like bone health (osteoporosis prevention), cardiovascular health, and cognitive function is paramount. Regular check-ups with the healthcare provider are crucial to monitor for potential complications and implement preventive measures.
Conclusion
Menopause in a 55-year-old client is a natural and expected event, but it's important to approach it with a holistic perspective. A comprehensive evaluation that includes a thorough history, physical examination, and relevant diagnostic tests is necessary to confirm the diagnosis and rule out other underlying conditions. Management should focus on alleviating symptoms, mitigating long-term health risks, and addressing the psychosocial impact of this significant life transition. By adopting a collaborative approach involving the client, healthcare provider, and potentially other specialists, a personalized management plan can be developed to improve the client’s quality of life during and after menopause. This approach will help improve the overall well-being of the client and allow for a smoother transition into this new phase of life. Regular follow-up appointments are crucial for ongoing monitoring and adjustment of the management plan as needed. Empowering the client with knowledge and support is key to a successful navigation of this important life stage.
Latest Posts
Latest Posts
-
Which Is An Example Of A Positive Incentive For Consumers
Mar 15, 2025
-
China And The Korean War Quick Check
Mar 15, 2025
-
Whem An Advanced Airway Is In Place
Mar 15, 2025
-
The National Safety Council Reports That Distracted Driving Leads To
Mar 15, 2025
-
Eric Files A Complaint Against Rugs R Us
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about A 55 Year Old Client Reports Cessation Of Menstrual Periods . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
