A Narrowing Or Stricture Of The Urethra Is Called Quizlet
Breaking News Today
Mar 31, 2025 · 7 min read
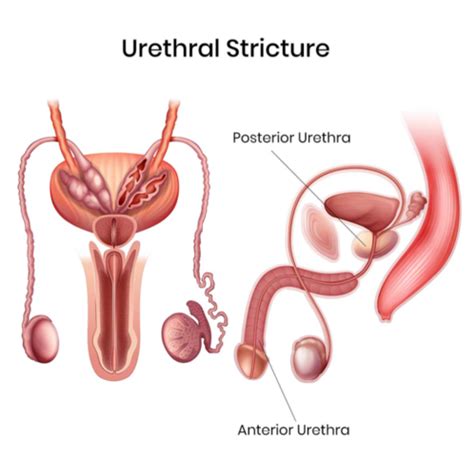
Table of Contents
A Narrowing or Stricture of the Urethra is Called: A Comprehensive Guide
A narrowing or stricture of the urethra is a condition known as urethral stricture. This comprehensive guide will delve deep into the intricacies of urethral stricture, covering its causes, symptoms, diagnosis, treatment options, and potential long-term effects. We'll also address frequently asked questions and provide valuable insights for those seeking a better understanding of this often-overlooked condition.
Understanding Urethral Stricture: What is it?
Urethral stricture is a condition characterized by the narrowing of the urethra, the tube that carries urine from the bladder to outside the body. This narrowing can occur anywhere along the urethra's length, from the bladder to the urethral meatus (the opening at the tip of the penis in men or the vaginal opening in women). The severity of the stricture can vary significantly, ranging from mild narrowing causing minimal symptoms to severe blockages requiring immediate medical attention. The condition primarily affects men, though women can also develop urethral strictures, albeit less frequently.
Causes of Urethral Stricture: Unraveling the Etiology
The development of urethral stricture can be attributed to a variety of factors, often stemming from injury or infection. Some of the most common causes include:
1. Trauma: A Leading Contributory Factor
Physical trauma to the urethra is a major culprit. This can include:
- Penile injuries: Straddle injuries (falling on a hard object astride the penis), penetrating injuries (gunshot wounds, stab wounds), and blunt force trauma can all lead to urethral damage and subsequent stricture formation.
- Surgical procedures: Prior pelvic surgeries, particularly those involving the prostate or bladder, can inadvertently damage the urethra, increasing the risk of stricture development.
- Catheterization: While necessary in certain medical situations, prolonged or repeated catheterization can cause urethral irritation and scarring, eventually leading to stricture.
2. Infections: The Inflammatory Pathway
Infections of the urethra, like urethritis, can cause inflammation and scarring, contributing to urethral narrowing. These infections are often sexually transmitted, underscoring the importance of safe sexual practices. Other infections, such as those involving the prostate (prostatitis), can also indirectly affect the urethra.
3. Inflammation and Scarring: The Body's Inappropriate Response
Chronic inflammation within the urethra can lead to the formation of scar tissue, resulting in a narrowed urethral lumen. This scarring process often follows trauma or infection, but can also be a consequence of underlying conditions.
4. Congenital Abnormalities: Present from Birth
In some cases, urethral strictures are present at birth (congenital). These are typically identified during infancy or early childhood.
5. Other contributing factors:
- Radiation therapy: Radiation treatment for pelvic cancers can damage the urethral tissue and lead to stricture formation.
- Certain medications: Some medications can have adverse effects on the urethra, potentially contributing to stricture.
Symptoms of Urethral Stricture: Recognizing the Warning Signs
The symptoms of urethral stricture vary depending on the severity of the narrowing. In mild cases, symptoms may be minimal or go unnoticed. However, as the stricture worsens, several characteristic symptoms can emerge:
- Weak or interrupted urine stream: This is often one of the earliest and most common symptoms. The stream may start strong but weaken or stop intermittently.
- Straining to urinate: Individuals may need to strain significantly to initiate or maintain the urine stream.
- Dribbling after urination: Incomplete bladder emptying leads to post-void dribbling.
- Frequent urination: The incomplete emptying of the bladder can result in a feeling of urgency and increased frequency of urination.
- Urinary tract infections (UTIs): Urethral stricture can make it more difficult to completely empty the bladder, increasing susceptibility to UTIs.
- Pain or burning during urination (dysuria): This can be a significant symptom, particularly in cases of associated infection.
- Blood in the urine (hematuria): This can indicate urethral irritation or damage.
- Retention of urine: In severe cases, the stricture can completely block the flow of urine, leading to urinary retention, a medical emergency requiring immediate treatment.
Diagnosis of Urethral Stricture: Identifying the Problem
Accurate diagnosis of urethral stricture is crucial for effective treatment. Several diagnostic procedures are employed:
- Physical examination: A physical examination, including palpation of the penis and perineum, may reveal areas of narrowing.
- Urine flow studies: These tests measure the rate and volume of urine flow to assess the severity of the obstruction.
- Retrograde urethrogram: A contrast dye is injected into the urethra, allowing visualization of the stricture on X-ray imaging. This is a key imaging method.
- Urethroscopy: A thin, flexible tube with a camera is inserted into the urethra, providing a direct visual examination of the stricture and surrounding tissue. This allows precise localization and assessment of the stricture's characteristics.
- Cystoscopy: A scope is inserted into the bladder to assess the bladder neck and its relationship to the stricture.
Treatment of Urethral Stricture: Restoring Normal Urinary Function
Treatment strategies for urethral stricture are tailored to the severity of the condition and the individual's overall health. Options include:
1. Dilation: Stretching the Narrowed Passage
Urethral dilation involves inserting progressively larger instruments into the urethra to gradually stretch the narrowed segment. This procedure can provide temporary relief but often requires repeated sessions.
2. Internal Urethrotomy: Surgical Incision
Internal urethrotomy involves making a surgical incision in the stricture to widen the urethral channel. This procedure is minimally invasive, performed using a specialized instrument inserted through the urethra. While effective, restenosis (re-narrowing) is possible.
3. Urethral Stents: Providing Internal Support
Urethral stents are small, flexible tubes placed within the urethra to keep it open. Stents can provide long-term relief but may require removal or replacement over time.
4. Urethral Reconstruction: Surgical Repair
For more severe or recurrent strictures, surgical reconstruction may be necessary. This procedure involves surgically excising the strictured segment of the urethra and replacing it with a graft from another part of the body or a synthetic material. This approach is more complex but often offers a more durable solution.
Long-Term Effects and Complications: Potential Challenges
If left untreated, urethral stricture can lead to several long-term complications:
- Kidney damage: Obstructed urine flow can increase pressure within the kidneys, potentially leading to damage over time.
- Bladder damage: Chronic urinary retention can damage the bladder and increase the risk of infections.
- Urinary incontinence: Damage to the urinary system can result in the inability to control urination.
- Sepsis: Severe infections related to urethral obstruction can lead to sepsis, a life-threatening condition.
Living with Urethral Stricture: Managing the Condition
Managing urethral stricture often involves a combination of lifestyle changes and medical interventions. Regular follow-up appointments with a urologist are crucial to monitor the condition's progression and manage any complications. Patients may need to adjust their fluid intake to maintain adequate hydration and reduce the risk of infections.
Frequently Asked Questions (FAQs): Addressing Your Concerns
Q: Is urethral stricture painful?
A: The level of pain varies depending on the severity of the stricture and the presence of infection. Some individuals experience minimal discomfort, while others report significant pain, particularly during urination.
Q: How common is urethral stricture?
A: Urethral stricture is more common in men than women. The exact prevalence is difficult to determine, but it's a significant urological concern.
Q: Can urethral stricture be prevented?
A: While not always preventable, practicing safe sex, avoiding trauma to the penis, and seeking prompt medical attention for any urinary problems can help reduce the risk.
Q: What is the prognosis for urethral stricture?
A: The prognosis depends on the severity of the stricture, the chosen treatment, and the individual's response to therapy. With appropriate management, many individuals can achieve long-term relief and improved urinary function.
Conclusion: Hope and Effective Management
Urethral stricture can be a challenging condition, but with the right diagnosis and treatment, many individuals can experience significant improvement in their urinary function and overall quality of life. Regular medical checkups, prompt attention to symptoms, and open communication with a healthcare provider are essential for effective management. Understanding the causes, symptoms, and treatment options empowers individuals to take proactive steps towards maintaining their health and well-being. Remember, early intervention is key in effectively managing urethral strictures and minimizing potential long-term complications.
Latest Posts
Latest Posts
-
You Should Use Low Beams Whenever You Can
Apr 02, 2025
-
El Edificio Del Museo Del Oro Tiene Seis Pisos
Apr 02, 2025
-
Compared To Terrestrial Planets Jovian Planets Are
Apr 02, 2025
-
Nurse Logic 2 0 Knowledge And Clinical Judgment Advanced Test
Apr 02, 2025
-
Which Of The Following Describe How To Communicate Pals
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about A Narrowing Or Stricture Of The Urethra Is Called Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
