A Nurse Is Evaluating A Client's Use Of A Cane
Breaking News Today
Mar 22, 2025 · 7 min read
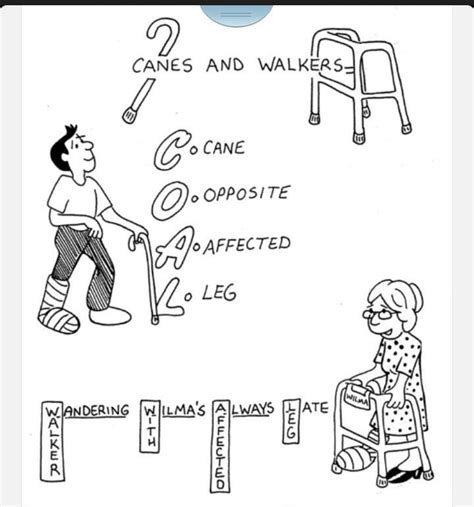
Table of Contents
A Nurse's Comprehensive Evaluation of Cane Use: Ensuring Patient Safety and Mobility
Nursing care extends beyond administering medications and monitoring vital signs; it encompasses a holistic assessment of a patient's functional abilities and overall well-being. A crucial aspect of this care involves evaluating a patient's use of assistive devices, such as canes, to ensure safe and effective mobility. This article delves into the comprehensive evaluation a nurse performs when assessing a client's cane usage, covering various aspects from initial observation to the development of an individualized care plan.
The Initial Assessment: Observation and Patient History
The evaluation begins with a thorough observation of the client's gait and cane technique. The nurse should note the following:
Gait Analysis:
- Posture: Is the client's posture erect and balanced, or are they stooped or leaning excessively? Poor posture can indicate underlying musculoskeletal issues or neurological deficits that impact cane use.
- Base of Support: Does the client maintain a stable base of support while walking? A narrow base suggests instability and an increased risk of falls.
- Step Length and Cadence: Are the steps even and consistent in length and timing? Uneven steps or a hesitant gait can indicate pain, weakness, or balance problems.
- Swing Phase: Does the client swing their leg freely or is there hesitancy or dragging of the foot? This observation provides insight into leg strength and coordination.
- Stance Phase: Does the client bear weight appropriately on their legs? Pain or weakness may cause them to favor one leg over the other.
- Use of Upper Extremities: Are the client's arms swinging naturally, or are they rigidly held? Restricted arm movement can be a sign of pain, neurological deficits, or other limitations.
Cane Technique:
- Cane Placement: Is the cane held correctly (typically in the hand opposite the affected leg)? Improper placement can compromise balance and increase fall risk.
- Cane Height: Is the cane adjusted to the appropriate height? An incorrectly sized cane can lead to improper weight bearing and strain on joints. The elbow should be flexed at approximately 30 degrees when the cane is used.
- Weight Bearing: Is the client distributing weight evenly between the cane and their legs? Over-reliance on the cane can weaken muscles and increase dependency.
- Use during Turns: Does the client use the cane appropriately during turns, ensuring stability? Difficulty turning indicates a potential need for additional support or gait training.
Patient History:
The nurse must gather comprehensive information about the client's medical history, including:
- Reason for Cane Use: Why does the client require a cane? This could be due to arthritis, stroke, weakness, balance problems, or other conditions. Understanding the underlying cause is crucial for effective intervention.
- Diagnosis and Medications: The client's medical diagnoses and current medications can influence gait and balance. Certain medications, for instance, can cause dizziness or orthostatic hypotension, increasing fall risk.
- Previous Falls: A history of falls is a significant risk factor. Understanding the circumstances of previous falls helps identify modifiable risk factors.
- Pain Level: Assessing the client's pain level is critical, as pain can significantly affect mobility and cane use.
- Cognitive Status: A client's cognitive abilities impact their understanding of cane use instructions and their ability to follow safety precautions.
- Vision and Hearing: Visual or auditory impairments can compromise safety and increase the risk of falls.
- Home Environment: An assessment of the client's home environment is crucial to identify potential hazards that could contribute to falls, even with proper cane use. This involves assessing floor surfaces, obstacles, and lighting.
Comprehensive Physical Examination
Following the initial observation and history, the nurse conducts a physical examination focusing on relevant systems:
- Musculoskeletal System: Range of motion, muscle strength, joint stability, and presence of pain or deformity are evaluated. This assessment informs the selection of an appropriate cane type and determines the need for physical therapy.
- Neurological System: Balance, coordination, reflexes, and sensation are assessed to detect any neurological deficits that might affect gait and cane use. This includes tests such as Romberg test and tandem gait.
- Cardiovascular System: Blood pressure and heart rate are monitored, particularly during ambulation, to identify any cardiovascular limitations affecting mobility. Orthostatic hypotension, a common issue in older adults, can increase fall risk.
- Sensory System: Visual acuity and hearing are tested, as diminished sensory function can affect the client's ability to navigate safely with a cane.
Cane Type and Assessment
The type of cane used is crucial. Different canes serve different purposes:
- Standard Cane: Provides basic support and stability.
- Quad Cane: Offers greater stability due to its four-point base.
- Offset Cane: Provides more support on one side, often used for clients with unilateral weakness or pain.
- Adjustable Cane: Allows for customized height adjustment to accommodate individual needs.
The nurse assesses if the client's current cane is appropriate for their needs and abilities. They may recommend a different type of cane if necessary. The height adjustment should always be checked and readjusted if necessary.
Developing an Individualized Care Plan
Based on the comprehensive evaluation, the nurse develops an individualized care plan that addresses the client's specific needs and challenges. This care plan might include:
- Gait Training: Instruction and practice in proper cane technique, including appropriate weight bearing, step length, and turning maneuvers.
- Strength Training Exercises: Exercises to improve muscle strength and endurance, which are crucial for safe and effective cane use.
- Balance Exercises: Exercises to enhance balance and coordination, reducing fall risk.
- Environmental Modifications: Recommendations for modifying the client's home environment to eliminate fall hazards. This might include installing grab bars, removing obstacles, and improving lighting.
- Assistive Devices: Assessment of other assistive devices that may be beneficial, such as walkers or wheelchairs, if the client's needs are beyond the capabilities of a cane.
- Fall Prevention Education: Education for the client and their family regarding fall prevention strategies.
- Referral to Physical Therapy: Referral to physical therapy for comprehensive gait training and strengthening exercises.
- Medication Review: Review of medications to identify any that might contribute to dizziness or falls.
- Regular Monitoring: Regular reassessment of the client's cane use and overall mobility to ensure the effectiveness of the care plan and to make adjustments as needed.
Documentation and Communication
Meticulous documentation is essential. The nurse must accurately record all aspects of the assessment, including:
- Client's gait and cane technique observations.
- Physical examination findings.
- Patient history and risk factors.
- Type of cane used.
- Interventions implemented.
- Client's response to interventions.
- Goals and outcomes.
- Recommendations for future care.
Effective communication with the client, family, and other healthcare providers is equally important. The nurse should explain the assessment findings, the rationale for the care plan, and the importance of adhering to safety recommendations. Collaboration with other members of the healthcare team, such as physical therapists and occupational therapists, is crucial for providing comprehensive care.
Ongoing Assessment and Intervention: A Continuous Process
Assessing a client's cane usage isn't a one-time event. It’s an ongoing process that requires continuous monitoring and adjustment. Regular reassessment allows the nurse to:
- Identify changes in the client's condition. The client's strength, balance, and overall mobility might improve or decline over time.
- Evaluate the effectiveness of interventions. Adjustments to the care plan may be necessary based on the client's progress.
- Prevent falls and promote safety. Early identification of potential problems can help prevent falls and maintain the client's independence.
- Promote Client Independence and Quality of Life: Empowering clients to use their assistive devices safely and effectively significantly impacts their overall independence, mobility, and quality of life.
By diligently following this comprehensive process, nurses can effectively evaluate a client's cane use, ensuring both safety and improved mobility. This thorough approach not only reduces fall risk but also enhances the client's overall quality of life and promotes a sense of independence. This holistic approach to mobility assessment is paramount in providing high-quality patient-centered care.
Latest Posts
Latest Posts
-
Compare Group Selection To Single Tree Selection
Mar 22, 2025
-
New York State Notary Exam Study Guide
Mar 22, 2025
-
Cpr Will Not Be Effective If The Patient Is
Mar 22, 2025
-
What Is The Marine Corps Order For Records Management
Mar 22, 2025
-
A New General Property And Casualty License
Mar 22, 2025
Related Post
Thank you for visiting our website which covers about A Nurse Is Evaluating A Client's Use Of A Cane . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
