A Patient Has A Rapid Irregular Wide Complex Tachycardia
Breaking News Today
Mar 13, 2025 · 7 min read
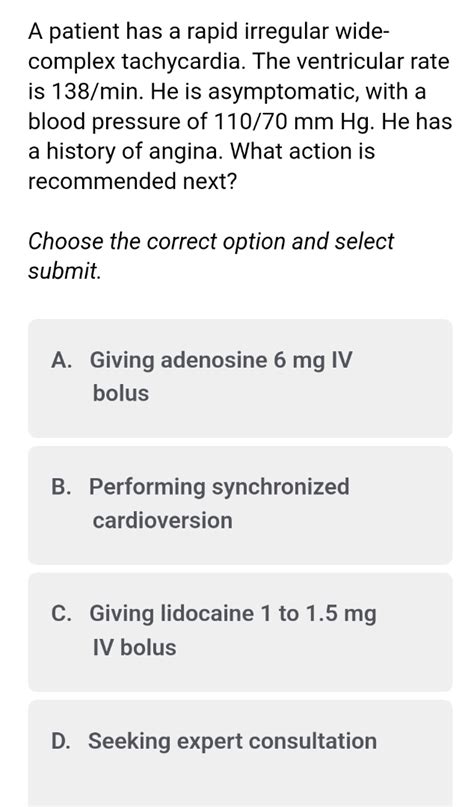
Table of Contents
A Patient Presents with Rapid Irregular Wide Complex Tachycardia: A Comprehensive Approach
Rapid irregular wide complex tachycardia (RIWCT) presents a diagnostic and therapeutic challenge in the emergency setting. The urgency stems from the potential for hemodynamic instability and the risk of underlying life-threatening conditions. This article delves into the differential diagnosis, investigative approaches, and management strategies for patients exhibiting this critical arrhythmia. We will explore the nuances of interpreting electrocardiograms (ECGs), emphasizing the importance of careful assessment and timely intervention.
Understanding the ECG Characteristics of RIWCT
The hallmark of RIWCT is precisely what its name implies: a rapid heart rate (typically >100 bpm), irregular rhythm, and wide QRS complexes (>120 ms). The irregularity distinguishes it from regular wide complex tachycardias, immediately broadening the differential diagnosis. The wide QRS complexes indicate that the impulse is not originating from the sinoatrial (SA) node and is likely being conducted through an abnormal pathway, often via the ventricles. This abnormal conduction can lead to significant hemodynamic compromise.
Key ECG Features to Analyze:
- Rate: Determine the ventricular rate. Is it extremely rapid, potentially leading to decreased cardiac output?
- Rhythm: Is the rhythm completely irregular, suggesting atrial fibrillation with aberrant conduction or other mechanisms? Look for any pattern or regularity within the irregularity.
- QRS Morphology: The shape and width of the QRS complexes provide crucial clues. Are they consistent throughout the rhythm, or do they vary? This can help differentiate between different etiologies.
- P Waves: Are P waves present? If present, are they related to the QRS complexes? The presence or absence of discernible P waves and their relationship to the QRS complexes are critical in differentiating supraventricular tachycardias with aberrant conduction from ventricular tachycardias.
- ST-T Wave Changes: Evaluate for any evidence of ischemia or infarction. ST-segment elevation or depression can indicate acute coronary syndrome, potentially a life-threatening complication.
Differential Diagnosis: Unraveling the Cause of RIWCT
The differential diagnosis of RIWCT is extensive and necessitates a systematic approach. The key is to differentiate between supraventricular tachycardias (SVTs) with aberrant conduction and ventricular tachycardias (VTs). This distinction is crucial because the management strategies differ significantly.
Supraventricular Tachycardias with Aberrant Conduction:
These arrhythmias originate above the ventricles (e.g., in the atria or atrioventricular (AV) node) but exhibit wide QRS complexes due to aberrant conduction through the ventricles. Common causes include:
- Atrial Fibrillation (AF) with Aberrant Conduction: This is a frequent cause of RIWCT. The chaotic atrial activity leads to irregular ventricular responses, resulting in a rapid, irregular, and wide complex rhythm. The irregularity is a key feature differentiating it from other wide complex tachycardias. The presence of fibrillation waves (f-waves) in the baseline may offer a clue, though they are often obscured by the rapid rate.
- Atrial Flutter with Aberrant Conduction: Similar to AF, atrial flutter involves rapid, regular atrial activity, but the ventricular response is irregular due to variable conduction through the AV node. This irregularity, coupled with wide QRS complexes, can mimic VT. The presence of characteristic flutter waves (sawtooth pattern) may be visible, especially with slower ventricular rates.
- AV Junctional Tachycardia with Aberrant Conduction: This originates in the AV junction and can exhibit aberrant conduction, leading to wide QRS complexes. While less common, it's important to consider.
Ventricular Tachycardias:
These arrhythmias originate in the ventricles, representing a significant threat due to their potential for hemodynamic instability and cardiac arrest. Causes include:
- Ischemic Heart Disease: Myocardial infarction (MI) is a major cause of VT. The damaged myocardial tissue can become irritable, leading to ectopic ventricular beats and sustained VT. The presence of ST-segment elevation or depression on the ECG is suggestive.
- Cardiomyopathy: Various forms of cardiomyopathy (dilated, hypertrophic, restrictive) can predispose to VT. Structural abnormalities in the myocardium create substrates for arrhythmogenesis.
- Electrolyte Imbalances: Disruptions in electrolytes, such as potassium, magnesium, and calcium, can significantly affect cardiac electrical activity and trigger VT.
- Congenital Long QT Syndrome: This inherited condition increases the risk of life-threatening arrhythmias, including VT and torsades de pointes (a polymorphic VT).
- Other Causes: Other less common causes include drug toxicity, valvular heart disease, myocarditis, and pulmonary embolism.
Diagnostic Approach: Investigating the Underlying Cause
Establishing the correct diagnosis is paramount for effective management. A systematic approach combining ECG analysis, clinical evaluation, and potentially further investigations is crucial.
1. Detailed History and Physical Examination:
A comprehensive history, focusing on cardiac risk factors (e.g., hypertension, diabetes, smoking, family history), symptoms (e.g., chest pain, shortness of breath, palpitations), and medication history is essential. A thorough physical examination, including blood pressure, heart rate, and auscultation for murmurs or other abnormal heart sounds, provides vital clinical clues.
2. ECG Interpretation and Further Analysis:
As previously discussed, meticulous analysis of the ECG is the cornerstone of diagnosis. Consider using advanced ECG interpretation techniques such as:
- Bundle Branch Block Criteria: Identify the presence of a bundle branch block (RBBB or LBBB). The presence of a pre-existing bundle branch block can significantly alter the appearance of a supraventricular arrhythmia, making it difficult to differentiate from VT.
- Axis Deviation: Analyze the QRS axis. Significant axis deviation can provide additional clues about the underlying cardiac structure and potential causes.
- Fusion Beats: The presence of fusion beats (combination of a normal and abnormal beat) is suggestive of VT.
- Capture Beats: The presence of capture beats (normal QRS complex interrupting the wide complex tachycardia) supports the diagnosis of SVT with aberrant conduction.
3. Additional Investigations:
If the ECG findings are inconclusive, further investigations may be necessary, including:
- Electrocardiographic Monitoring: Continuous ECG monitoring provides a more complete picture of the arrhythmia, including the duration and frequency of episodes.
- Echocardiography: This imaging technique provides information about cardiac structure and function, aiding in the identification of cardiomyopathy, valvular heart disease, and other structural abnormalities that might predispose to RIWCT.
- Cardiac Catheterization: This invasive procedure can be used to identify coronary artery disease, which might be responsible for VT in the context of an acute coronary syndrome.
- Electrophysiology Study (EPS): EPS is an invasive electrophysiological study that can pinpoint the origin of the arrhythmia and assess the response to antiarrhythmic drugs. This is often reserved for patients with recurrent or hemodynamically significant RIWCT.
- Laboratory Investigations: Blood tests should assess electrolytes (potassium, magnesium, calcium), cardiac biomarkers (troponin), and thyroid function.
Management Strategies: Stabilizing the Patient and Addressing the Underlying Cause
Management of RIWCT is determined by the hemodynamic status of the patient and the suspected underlying cause.
1. Immediate Stabilization:
If the patient is hemodynamically unstable (e.g., hypotensive, syncopal), immediate cardioversion is indicated. Synchronized cardioversion delivers a shock to the heart that is synchronized with the QRS complex, effectively terminating the tachycardia.
2. Pharmacological Management:
If the patient is hemodynamically stable, pharmacological management may be attempted. The choice of medication depends on the suspected cause of the RIWCT. Amiodarone is often the drug of choice due to its broad spectrum of activity, effectiveness in both SVT and VT, and relatively low risk of adverse effects. Other medications such as procainamide, lidocaine, and adenosine might be used based on the clinical scenario and suspected etiology. The use of these medications should be guided by a physician experienced in the management of arrhythmias.
3. Long-Term Management:
Once the acute episode is managed, long-term management focuses on preventing recurrence. This may involve:
- Anticoagulation: If AF is identified as the cause, long-term anticoagulation is typically recommended to prevent thromboembolic events.
- Antiarrhythmic Medications: Depending on the underlying cause and risk of recurrence, long-term antiarrhythmic medication may be required.
- Catheter Ablation: For patients with recurrent, symptomatic RIWCT, catheter ablation may be considered. This procedure involves destroying the aberrant conduction pathways responsible for the arrhythmia.
- Cardiac Devices: In patients at high risk of sudden cardiac death, implantable cardioverter-defibrillators (ICDs) may be indicated to provide life-saving shocks should VT occur.
Conclusion: A Multifaceted Approach to a Critical Arrhythmia
Rapid irregular wide complex tachycardia presents a complex diagnostic and therapeutic challenge. A systematic approach integrating detailed ECG analysis, clinical assessment, and potentially further investigations is crucial for identifying the underlying cause and implementing appropriate management strategies. The urgency of this arrhythmia underscores the importance of prompt recognition, timely intervention, and effective long-term management to improve patient outcomes and prevent life-threatening complications. The information provided herein is for educational purposes only and should not be considered medical advice. Always consult with a healthcare professional for diagnosis and treatment of any medical condition.
Latest Posts
Latest Posts
-
How Is A Respirometer Used To Measure Fermentation
May 09, 2025
-
Regarding The Magna Carta Which Statement Is False
May 09, 2025
-
How Should The Sonata Form Be Viewed
May 09, 2025
-
What Is The Minimal Acceptable Vision For Driving In Georgia
May 09, 2025
-
Match The Type Of Rock Dating With Its Description
May 09, 2025
Related Post
Thank you for visiting our website which covers about A Patient Has A Rapid Irregular Wide Complex Tachycardia . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.