A Patient's Refusal Of Ems Treatment And/or Transport Must Be
Breaking News Today
Mar 26, 2025 · 6 min read
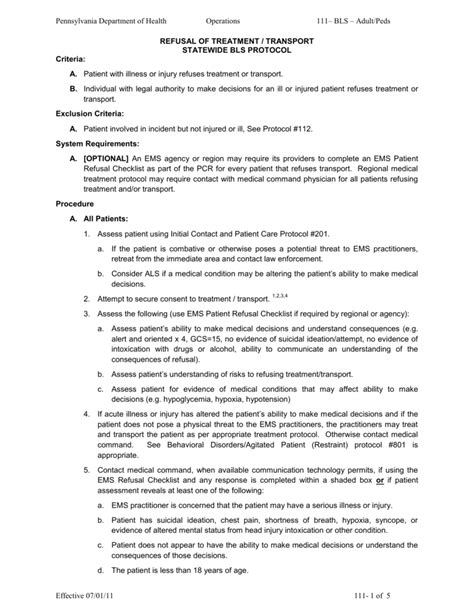
Table of Contents
A Patient's Refusal of EMS Treatment and/or Transport: Understanding the Legal and Ethical Implications
Emergency Medical Services (EMS) personnel routinely encounter situations where patients refuse treatment or transport. This complex scenario necessitates a delicate balance between respecting patient autonomy and ensuring their safety and well-being. This article delves into the legal and ethical considerations surrounding a patient's refusal of EMS treatment and/or transport, exploring the crucial steps EMS providers must take to navigate these challenging situations effectively and responsibly.
Understanding Patient Autonomy and Informed Consent
The cornerstone of this discussion is patient autonomy, the right of competent adults to make decisions about their own medical care, even if those decisions seem unwise to others. This right is underpinned by the principle of informed consent. For a patient's refusal to be valid, they must be:
-
Competent: This means the patient possesses the capacity to understand the nature of their condition, the proposed treatment (or lack thereof), the potential risks and benefits of treatment and refusal, and the potential consequences of refusing treatment. Factors affecting competency include age, mental state (including intoxication), and cognitive impairment. A minor's refusal is generally not considered valid unless they are an emancipated minor or there's a specific legal exception.
-
Informed: The patient must receive clear, concise, and understandable information about their condition, the recommended treatment options, and the potential consequences of accepting or refusing treatment. This includes potential risks and benefits of both choices. Information should be provided in a language the patient understands, with the aid of interpreters if necessary.
-
Voluntary: The decision to refuse treatment must be made freely and without coercion, duress, or undue influence from others. EMS providers must avoid pressuring the patient into accepting treatment.
Documentation: The Cornerstone of a Valid Refusal
Meticulous documentation is paramount in cases of treatment or transport refusal. This documentation serves as crucial evidence should any legal or ethical questions arise later. Comprehensive documentation should include:
-
Patient Identification: Full name, date of birth, address, and any other relevant identifiers.
-
Assessment Findings: A detailed account of the patient's chief complaint, vital signs, and physical examination findings. This provides context for the refusal decision.
-
Explanation of Treatment Options: A clear description of the recommended treatment and transport options, including potential benefits and risks of accepting treatment versus refusing.
-
Patient's Understanding: A statement confirming that the patient understands the information provided, including the potential consequences of refusal. This might involve repeating information back to the provider or using a teach-back method.
-
Patient's Refusal: A clear and concise statement from the patient indicating their refusal of treatment or transport. Ideally, this is documented in the patient's own words, or through a witnessed signature on a refusal form.
-
Witness Information: If possible, include the name and contact information of any witnesses to the refusal.
-
Patient's Mental Status: A detailed assessment of the patient's cognitive state and mental capacity, noting any signs of intoxication, confusion, or impairment.
-
EMS Provider's Assessment: The provider's professional opinion regarding the patient's competency to refuse treatment and their assessment of the risks associated with the refusal.
-
Photographs or Video: In some situations, photographs or video documentation of the patient's condition and the surrounding circumstances may be beneficial. However, ethical and legal considerations regarding patient privacy must be carefully adhered to.
-
Contact Information: Include contact information for any family members or other individuals who may be able to provide support or assistance.
Legal Considerations and Potential Liabilities
While respecting patient autonomy is vital, EMS providers also bear a responsibility to ensure patient safety. This creates a potential legal gray area. Improper handling of a patient refusal can lead to liability issues for both the individual providers and the EMS agency.
Potential legal challenges might arise if:
-
The patient is deemed incompetent: If the patient lacked the capacity to make an informed decision, the refusal may not be legally valid.
-
The refusal was not truly voluntary: Evidence of coercion or undue influence could invalidate the refusal.
-
The provider failed to adequately document the refusal: Poor documentation can weaken the provider's defense against potential legal claims.
-
The provider failed to provide appropriate information: Insufficient information given to the patient may invalidate the consent.
-
The patient's condition deteriorated significantly after refusal: While not automatically leading to liability, this situation requires careful review of the documentation to ensure appropriate care was offered and the refusal was properly documented and understood.
Ethical Considerations: Balancing Autonomy and Beneficence
Beyond the legal aspects, ethical dilemmas abound. The principles of beneficence (acting in the patient's best interest) and non-maleficence (avoiding harm) often conflict with patient autonomy. EMS providers must carefully consider the patient's best interests while simultaneously respecting their right to self-determination.
This often involves difficult questions like:
-
How much risk is acceptable? What level of risk to the patient is acceptable before intervening despite their refusal?
-
What constitutes undue influence? Drawing the line between offering information and applying pressure is crucial.
-
How do you handle a refusal when you suspect a patient is suicidal or homicidal? Specific protocols and legal frameworks guide these circumstances.
-
How do you deal with a refusal from a patient who appears to lack capacity but is still insistent? This requires careful assessment and potentially involving other professionals, such as law enforcement or a psychiatrist.
Strategies for Managing Patient Refusals
To effectively manage patient refusals, EMS providers should employ several strategies:
-
Thorough Assessment: Conduct a comprehensive assessment to determine the patient's condition and competency.
-
Clear and Concise Communication: Explain treatment options in plain language, answering questions patiently and thoroughly. Use visual aids if necessary.
-
Documentation: Maintain meticulous documentation of every aspect of the interaction.
-
Multiple Attempts: Attempt to persuade the patient to reconsider their decision, but avoid coercion.
-
Witnessing the Refusal: Obtain the signatures of multiple witnesses to the refusal.
-
Involving Family or Guardians: Seek input from family members or guardians when appropriate and permissible by law.
-
Seeking Medical Control: Consult medical control or other appropriate professionals for guidance in complex cases.
-
Consideration of Alternative Care Options: Explore alternative options like arranging for a follow-up appointment with a physician or providing information on community resources.
-
Consideration of Legal Intervention: In certain circumstances, when there is evidence of an imminent threat to the patient or others, legal intervention might be necessary (e.g., involuntary commitment).
Conclusion: Navigating a Complex Landscape
Managing a patient's refusal of EMS treatment and transport presents a multifaceted challenge requiring a delicate balance between legal obligations, ethical principles, and the patient's right to self-determination. Thorough assessment, clear communication, meticulous documentation, and a commitment to respecting patient autonomy are essential elements in navigating this complex landscape responsibly and effectively. EMS providers must receive adequate training to effectively manage these situations, ensuring both patient safety and adherence to legal and ethical standards. Continual education and the development of standardized protocols are vital to promoting consistent and best practices in the face of patient refusals. The ultimate goal is to provide the highest quality of care while safeguarding both the patient and the provider.
Latest Posts
Latest Posts
-
Guess The Movie With Emojis With Answers
Mar 29, 2025
-
Which Of These Is Not A Qualifying Event For Medicare
Mar 29, 2025
-
La Primera Pareja Lleva Ropa De Color Negro
Mar 29, 2025
-
What Makes A Battery Low Maintenance Or Maintenance Free
Mar 29, 2025
-
An Example Of A Two Point Violation Includes Reckless Driving
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about A Patient's Refusal Of Ems Treatment And/or Transport Must Be . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
