An Audit Is Defined By Ich E6 As
Breaking News Today
Mar 19, 2025 · 7 min read
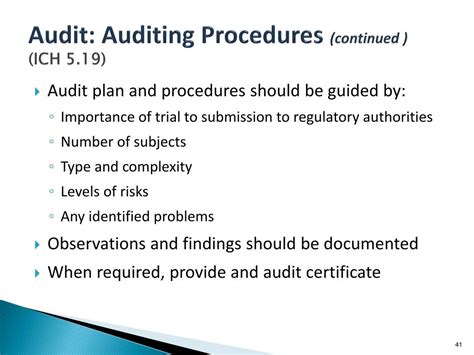
Table of Contents
An Audit Defined by ICH E6: A Comprehensive Guide to Good Clinical Practice (GCP) Compliance
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) E6 guideline, "Good Clinical Practice (GCP) for Trials on Pharmaceutical Products," provides a fundamental framework for conducting ethical and scientifically sound clinical trials. Central to maintaining GCP compliance is the concept of the audit. This article will delve deep into ICH E6's definition of an audit, exploring its purpose, scope, process, and vital importance in ensuring the integrity of clinical research.
What is an Audit According to ICH E6?
ICH E6 doesn't explicitly offer a single, concise definition of an audit. Instead, it implicitly defines it through its description of the audit process and its objectives. Essentially, an audit within the context of ICH E6 is a systematic and independent examination of trial-related activities and documentation to assess compliance with the protocol, GCP, and applicable regulatory requirements. This assessment verifies whether the trial was conducted, recorded, and reported according to the standards set forth to protect the rights, safety, and well-being of human subjects and ensure the integrity of the clinical trial data.
The emphasis on systematic and independent is crucial. Systematic implies a planned and structured approach, following a pre-defined methodology. Independence means the audit should be conducted by individuals free from any bias or influence that might compromise the objectivity of the assessment. This often involves using external auditors or individuals within the organization who are not directly involved in the specific trial being audited.
The Purpose of an Audit in Clinical Trials
The primary purpose of an audit, as implied by ICH E6, is to ensure the quality and integrity of the clinical trial data. This is achieved through several key objectives:
1. Verification of Compliance:
Audits verify adherence to the trial protocol, GCP guidelines, and all relevant regulatory requirements. This includes reviewing documentation related to subject recruitment, informed consent, data management, safety reporting, and more.
2. Identification of Deviations and Non-Compliance:
A key goal is to identify any deviations from the protocol, GCP, or regulations. These deviations, even minor ones, can impact the overall reliability and validity of the trial results. The audit process aims to uncover these issues, allowing for corrective actions.
3. Assessment of Investigator Site Performance:
Audits evaluate the performance of investigators and their sites in managing the trial. This involves assessing the site's adherence to the protocol, its ability to maintain accurate records, and its capacity to protect the rights and safety of study participants.
4. Ensuring Data Integrity:
Data integrity is paramount in clinical trials. Audits ensure the accuracy, completeness, consistency, and reliability of the data collected. This includes examining data handling procedures, data entry methods, and data validation processes.
5. Risk Mitigation:
By proactively identifying and addressing potential problems, audits contribute significantly to risk mitigation. Early detection of issues prevents the escalation of problems that could jeopardize the trial's integrity and compromise the safety of subjects.
The Scope of an Audit: What's Included?
The scope of an audit can vary depending on several factors, including the size and complexity of the trial, the specific concerns, and the regulatory requirements. However, a typical audit will encompass the following:
1. Trial Master File (TMF):
A comprehensive review of the TMF is a cornerstone of any GCP audit. The TMF contains all essential trial-related documents, providing a complete audit trail of the study's conduct. Auditors scrutinize the TMF's completeness, accuracy, and organization.
2. Investigator Site Files:
These files contain site-specific documentation related to subject recruitment, data collection, and safety reporting. Auditors meticulously examine these files to assess compliance with the protocol and GCP.
3. Case Report Forms (CRFs):
CRFs are the primary source of data in a clinical trial. Auditors review the CRFs for completeness, accuracy, consistency, and adherence to data collection procedures.
4. Informed Consent Documents:
The audit process verifies that informed consent was obtained from all subjects appropriately and that their rights were protected throughout the trial.
5. Safety Reporting Documentation:
This includes all documentation related to adverse events, serious adverse events, and other safety-related issues. Auditors ensure that adverse events were reported promptly and accurately.
6. Protocol and Other Study Documents:
Auditors review the trial protocol, amendments, and other essential documents to ensure that all study activities were conducted as planned and in accordance with approved documentation.
The Audit Process: A Step-by-Step Guide
The audit process generally follows these key steps:
1. Planning and Preparation:
This phase involves defining the audit scope, objectives, and methodology. A detailed audit plan should be developed, specifying the documents to be reviewed, the personnel involved, and the timeframe for the audit.
2. On-Site Visit (if applicable):
For many audits, an on-site visit to the investigator site is required. During the visit, auditors will review documents, interview personnel, and observe trial-related activities.
3. Document Review:
A thorough review of all relevant documents is crucial. This involves examining the completeness, accuracy, consistency, and conformity of the documentation to the protocol and GCP requirements.
4. Interviewing Personnel:
Interviews with key personnel, including investigators, study coordinators, and data managers, are essential to obtain additional information and clarify any discrepancies identified during the document review.
5. Report Writing:
Upon completion of the audit, a detailed audit report is prepared. This report summarizes the findings, identifies any deviations from GCP or the protocol, and provides recommendations for corrective actions.
6. Follow-up and Corrective Actions:
Following the audit, the sponsor and the investigator site implement corrective actions to address any identified deviations or deficiencies. A follow-up audit may be conducted to verify that corrective actions have been implemented effectively.
Importance of Audits in Maintaining GCP Compliance
Audits are critical for maintaining GCP compliance and ensuring the trustworthiness of clinical trial results. They provide several key benefits:
- Protecting the rights and safety of human subjects: Audits help to verify that subjects are adequately protected throughout the trial.
- Ensuring data integrity: Audits maintain the accuracy, reliability, and consistency of the data generated, leading to credible trial results.
- Identifying and correcting errors: Audits help uncover and address errors or inconsistencies that could compromise the trial's validity.
- Improving trial conduct: Audits contribute to a better understanding of best practices in conducting clinical trials.
- Compliance with regulatory requirements: Audits demonstrate adherence to national and international regulations, minimizing the risk of regulatory sanctions.
- Maintaining sponsor credibility: Audits protect the reputation and credibility of the sponsor and its associated organizations.
Types of Audits
While ICH E6 doesn't explicitly categorize audits, several types are commonly employed:
- Pre-audit: A pre-audit is a preliminary review conducted before a full-scale audit to identify potential areas of concern.
- Full-scale audit: This comprehensive audit assesses all aspects of the trial.
- Follow-up audit: A follow-up audit verifies that corrective actions taken after a previous audit were implemented effectively.
- Internal audit: Conducted by an organization’s internal audit team.
- External audit: Conducted by an independent third-party auditing firm.
- Regulatory audit: Conducted by a regulatory authority.
Conclusion: Audits - A Cornerstone of Trustworthy Clinical Research
ICH E6 emphasizes the critical role of audits in maintaining the integrity of clinical trials. While not explicitly defining an audit, the guideline underscores the need for systematic, independent examinations to ensure compliance with GCP and regulatory requirements. The audit process, from planning and preparation to follow-up and corrective actions, is essential for protecting human subjects, ensuring data integrity, and fostering public trust in clinical research. Regular audits are not simply a formality; they are a cornerstone of trustworthy clinical research and a commitment to the highest ethical and scientific standards. Understanding and implementing robust audit processes are vital for all stakeholders involved in clinical trials.
Latest Posts
Latest Posts
-
The James Lange Theory Of Emotion States That
Mar 19, 2025
-
At Which Osi Model Layer Does A Media Converter Operate
Mar 19, 2025
-
Sabe 1 Of 1 Donde Hay Un Buen Restaurante
Mar 19, 2025
-
Which Option Is An Example Of A Complex Sentence
Mar 19, 2025
-
Hans Selyes Definition Of Stress Is Considered
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about An Audit Is Defined By Ich E6 As . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
