Antibiotics Can Lead To Septic Shock If Used To Treat
Breaking News Today
Mar 19, 2025 · 6 min read
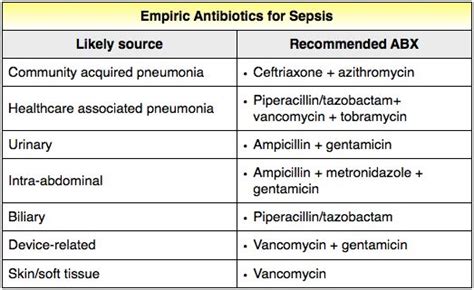
Table of Contents
Antibiotics: A Double-Edged Sword – Understanding the Risk of Septic Shock
Antibiotics, our stalwart allies in the fight against bacterial infections, are a cornerstone of modern medicine. They've dramatically reduced mortality rates from previously deadly diseases. However, like many powerful tools, antibiotics possess a double edge. Improper use, particularly in treating inappropriate conditions, can lead to severe complications, including the life-threatening condition known as septic shock. This article delves into the complex relationship between antibiotic use and septic shock, exploring the mechanisms, risk factors, and preventative measures.
Understanding Septic Shock: A Cascade of Failure
Septic shock is a life-threatening condition arising from the body's overwhelming response to an infection. It's not the infection itself that directly causes septic shock, but rather the body's dysregulated immune response to the infection. This response triggers a cascade of events:
-
Infection: The initial trigger is a bacterial, fungal, viral, or parasitic infection. This infection can originate anywhere in the body – from a simple wound to a severe pneumonia.
-
Inflammation: The body's immune system recognizes the infection and launches an inflammatory response. This is a normal and necessary process, designed to eliminate the pathogen.
-
Systemic Inflammatory Response Syndrome (SIRS): In septic shock, the inflammatory response becomes dysregulated, escalating beyond its intended purpose. SIRS is characterized by two or more of the following: fever or hypothermia, tachycardia (rapid heart rate), tachypnea (rapid breathing), and leukocytosis (increased white blood cell count).
-
Organ Dysfunction: The uncontrolled inflammation damages blood vessels, leading to widespread leakage of fluids into tissues. This causes a drop in blood pressure (hypotension), reducing blood flow to vital organs. This organ dysfunction can affect the heart, lungs, kidneys, brain, and other systems.
-
Septic Shock: Septic shock is defined as sepsis-induced hypotension persisting despite adequate fluid resuscitation. This indicates a severe circulatory collapse, requiring immediate medical intervention. The mortality rate of septic shock is significant, highlighting the urgency of its management.
How Antibiotics Contribute to Septic Shock: The Paradoxical Risk
The seemingly paradoxical connection between antibiotics and septic shock lies in the complexities of the immune response and the potential for antibiotic-associated complications. While antibiotics are designed to kill bacteria, their use can sometimes exacerbate the situation, leading to septic shock in several ways:
-
Antibiotic-Associated Diarrhea and Clostridium difficile (C. difficile) Infection: Broad-spectrum antibiotics, which target a wide range of bacteria, can disrupt the natural balance of gut flora. This disruption allows opportunistic pathogens, such as C. difficile, to proliferate. C. difficile infection, also known as C. difficile colitis, can cause severe diarrhea, leading to dehydration, sepsis, and ultimately, septic shock. The overgrowth of this bacteria highlights the critical role of the microbiome in preventing potentially lethal infections.
-
Antibiotic Resistance: The widespread use of antibiotics has fueled the rise of antibiotic-resistant bacteria. These resistant bacteria are harder to treat, leading to prolonged infections and an increased risk of sepsis and septic shock. This emphasizes the critical need for judicious antibiotic use and the development of new antimicrobial agents.
-
Immune Dysregulation: Some studies suggest that antibiotics can interfere with the body's immune response, potentially impairing its ability to effectively combat infections. This immune dysregulation might contribute to a more severe inflammatory response and increase the risk of progressing to septic shock. The complex interaction between antibiotics and the immune system is an area of ongoing research.
-
Treatment of inappropriate conditions: Prescribing antibiotics for viral infections is ineffective and can contribute to the development of antibiotic resistance and the potential for further complications. Using antibiotics in cases of self-limiting bacterial infections, where the body can naturally clear the infection without antibiotics, also contributes to unnecessary antibiotic use and related risks.
-
Adverse Reactions: While rare, certain antibiotics can trigger allergic reactions or other adverse effects. These effects can further compromise the body's immune response, increasing susceptibility to sepsis and septic shock.
Risk Factors for Septic Shock after Antibiotic Treatment
Several factors increase the risk of developing septic shock after receiving antibiotic treatment. These include:
-
Underlying medical conditions: Individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or diabetes, are at higher risk. This group will often require prophylactic antibiotics before certain procedures but can have more serious complications.
-
Age: Both the very young and the elderly are at increased risk due to their less robust immune systems.
-
Severity of the initial infection: Severe or invasive infections are more likely to progress to sepsis and septic shock.
-
Presence of indwelling devices: Catheters, intravenous lines, and other indwelling medical devices provide entry points for infection.
-
Hospitalization: Hospital-acquired infections are a significant source of sepsis and septic shock.
Preventing Septic Shock: A Multi-pronged Approach
Preventing septic shock requires a multi-faceted approach focusing on appropriate antibiotic use and managing underlying conditions.
-
Judicious Antibiotic Use: This is paramount. Antibiotics should only be used when necessary, based on a proper diagnosis of a bacterial infection. The focus on stewardship programs should be highlighted for a reduction of unnecessary prescriptions.
-
Appropriate Antibiotic Choice: The choice of antibiotic should be based on the specific pathogen involved and its susceptibility profile. Broad-spectrum antibiotics should be used only when necessary, to minimize disruption of the gut flora.
-
Infection Control Practices: Strict adherence to infection control protocols in healthcare settings is essential to prevent healthcare-associated infections. This includes proper hand hygiene, sterilization of equipment, and isolation of infected patients.
-
Early Diagnosis and Treatment of Infection: Early detection and treatment of infections are crucial in preventing progression to sepsis and septic shock. Symptoms should not be overlooked.
-
Managing Underlying Conditions: Proper management of chronic conditions such as diabetes and HIV/AIDS can help strengthen the immune system and reduce the risk of severe infections.
-
Vaccination: Vaccinations against common pathogens can significantly reduce the risk of bacterial infections.
-
Monitoring for Sepsis: Healthcare professionals should carefully monitor patients for signs and symptoms of sepsis, especially those at high risk. Prompt recognition and treatment are essential for improving outcomes.
The Role of Healthcare Professionals in Sepsis Prevention
Healthcare professionals play a crucial role in preventing septic shock. This includes:
- Accurate Diagnosis: Making an accurate diagnosis to determine whether antibiotics are necessary.
- Appropriate Antibiotic Prescribing: Prescribing antibiotics only when necessary and selecting the most appropriate antibiotic based on susceptibility testing.
- Infection Control: Maintaining strict infection control practices to minimize the risk of healthcare-associated infections.
- Patient Education: Educating patients about the importance of hand hygiene and other infection prevention measures.
- Early Recognition and Treatment of Sepsis: Prompt recognition of the signs and symptoms of sepsis and immediate treatment.
Conclusion: A Call for Vigilance and Responsible Antibiotic Use
Antibiotics are indispensable tools in fighting bacterial infections. However, their improper use can lead to severe complications, including septic shock. The risk is compounded by the rise of antibiotic resistance and the complex interplay between antibiotics and the immune system. A multi-pronged approach, including judicious antibiotic use, strict infection control practices, and early recognition and treatment of sepsis, is essential to mitigate this risk and improve patient outcomes. Understanding this intricate relationship between antibiotics and septic shock empowers individuals and healthcare professionals alike to make informed decisions and safeguard against this life-threatening condition. The future of combating bacterial infections rests on a balanced approach that prioritizes responsible antibiotic stewardship while simultaneously advancing research in new antimicrobial therapies. This collective effort will be crucial in minimizing the risks associated with antibiotic use and ultimately saving lives.
Latest Posts
Latest Posts
-
Which Of These Are Examples Of Business Analytics
Mar 19, 2025
-
The Custodian Of A Company Asset Should
Mar 19, 2025
-
What Does Nick Think Of Gatsby After Meeting Him
Mar 19, 2025
-
Explain How Changes In Land Use Can Impact An Ecosystem
Mar 19, 2025
-
Ap Gov Unit 1 Progress Check Mcq
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Antibiotics Can Lead To Septic Shock If Used To Treat . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
