Assessment Of A Patient With Hypoglycemia Will Most Likely Reveal
Breaking News Today
Mar 19, 2025 · 6 min read
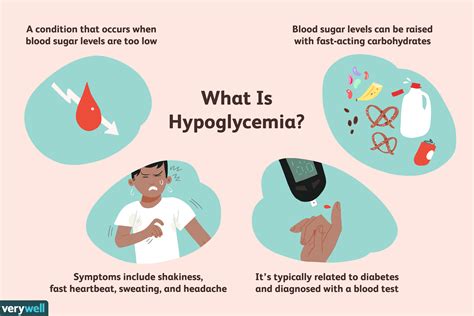
Table of Contents
Assessment of a Patient with Hypoglycemia Will Most Likely Reveal: A Comprehensive Guide
Hypoglycemia, characterized by abnormally low blood glucose levels, presents a significant diagnostic and therapeutic challenge. Understanding its diverse manifestations is crucial for prompt and effective management. This article delves into the comprehensive assessment of a patient presenting with hypoglycemia, exploring the likely findings across various systems and emphasizing the importance of a thorough approach.
Initial Presentation: Recognizing the Signs and Symptoms
The initial presentation of hypoglycemia is highly variable, depending on the rapidity of onset, the severity of the hypoglycemia, and the individual's pre-existing conditions and medications. A patient might present with classic symptoms or a more insidious, atypical presentation, making accurate diagnosis challenging.
Classic Symptoms of Hypoglycemia:
These are typically seen with a rapid drop in blood glucose levels:
-
Neuroglycopenic Symptoms: These arise from insufficient glucose supply to the brain. They include:
- Neurological: Confusion, dizziness, headache, blurred vision, slurred speech, incoordination, seizures, loss of consciousness.
- Autonomic: Sweating, palpitations, tremors, anxiety, hunger, pallor.
-
Severity: The severity of symptoms correlates with the degree and speed of blood glucose decline. Mild hypoglycemia might manifest as mild anxiety and hunger, while severe hypoglycemia can lead to seizures, coma, and even death.
Atypical Presentations of Hypoglycemia:
In some individuals, especially those with chronic hypoglycemia or those on certain medications, the classic symptoms may be absent or attenuated. This includes:
- Masked Hypoglycemia: This is particularly problematic as patients may not experience the usual warning signs. They might present with nonspecific symptoms like fatigue, weakness, cognitive impairment, or behavioral changes, leading to delayed diagnosis and management.
- Older Adults: In older adults, the presentation might be subtle and include confusion, falls, or altered mental status, often mistaken for other neurological conditions.
- Patients with Autonomic Neuropathy: Patients with diabetes and associated autonomic neuropathy may lack the typical adrenergic symptoms (sweating, palpitations) making diagnosis more challenging.
Physical Examination: Clues from the Head-to-Toe Assessment
A comprehensive physical examination is pivotal in assessing a patient with suspected hypoglycemia. The examiner should meticulously evaluate several aspects:
Vital Signs:
- Tachycardia: Rapid heart rate is a common finding due to the sympathetic nervous system's response to low glucose.
- Hypotension: Low blood pressure can occur, particularly in severe cases.
- Tachypnea: Increased respiratory rate may be present due to the body's attempt to compensate for the energy deficit.
Neurological Examination:
- Mental Status: Assess the patient's level of consciousness, orientation, and cognitive function. This is critical to gauge the severity of neurological involvement.
- Cranial Nerves: Evaluate cranial nerve function for any deficits indicative of neurological compromise.
- Motor Strength and Coordination: Assess for weakness, tremors, and incoordination.
Other Systems:
- Skin: Check for pallor, diaphoresis (sweating), and cool, clammy skin.
- Cardiovascular: Listen to the heart sounds for any abnormalities.
- Respiratory: Assess respiratory rate, rhythm, and depth.
- Gastrointestinal: Inquire about nausea, vomiting, or abdominal discomfort.
Laboratory Investigations: Confirming the Diagnosis and Identifying the Cause
The diagnosis of hypoglycemia relies heavily on laboratory investigations. While clinical findings are crucial, they are not sufficient to confirm the diagnosis.
Blood Glucose Measurement:
- Capillary Blood Glucose: A rapid bedside test is the first step in confirming hypoglycemia. However, it's crucial to remember that capillary blood glucose might slightly differ from venous blood glucose.
- Venous Blood Glucose: A venous blood glucose measurement is necessary for accurate confirmation and documentation. A value consistently below 70 mg/dL (3.9 mmol/L) is typically considered hypoglycemia, although the threshold may vary slightly depending on individual circumstances and institutional protocols.
Further Investigations to Determine the Underlying Cause:
Once hypoglycemia is confirmed, further investigations are essential to identify the underlying cause, which can be complex and multifaceted. These investigations might include:
- Insulin and C-peptide Levels: These are crucial in differentiating between various causes of hypoglycemia, especially in cases of suspected insulinoma. Elevated insulin with suppressed C-peptide suggests exogenous insulin administration or insulinoma.
- Blood Ketones: Assessing ketone levels helps distinguish between hypoglycemia caused by starvation or insulin-induced hypoglycemia.
- Liver Function Tests (LFTs): These may be helpful in identifying liver dysfunction as a possible cause.
- Renal Function Tests (RFTs): These are useful in assessing renal function, especially in patients with renal failure or those taking certain medications.
- Cortisol and Growth Hormone Levels: These hormonal assessments aid in evaluating adrenal insufficiency or growth hormone deficiency, which can lead to hypoglycemia.
- Fasting Blood Glucose: To assess for fasting hypoglycemia, a 72-hour fast (under medical supervision) may be needed in some cases.
- Oral Glucose Tolerance Test (OGTT): This helps to diagnose reactive hypoglycemia, where hypoglycemia occurs after consuming carbohydrates.
- Imaging Studies: In cases of suspected insulinoma, imaging studies like CT scan or MRI of the pancreas are essential to locate the tumor.
Differential Diagnosis: Considering Other Possibilities
It's essential to remember that hypoglycemia mimics many other conditions. The differential diagnosis should include:
- Neurological Disorders: Stroke, seizure, syncope, brain tumor, encephalitis.
- Cardiovascular Conditions: Cardiac arrhythmias, heart failure.
- Endocrine Disorders: Adrenal insufficiency, hypothyroidism, hypopituitarism.
- Medication Side Effects: Certain medications can induce hypoglycemia.
- Alcohol Intoxication: Alcohol can lead to hypoglycemia, particularly in individuals with limited glycogen stores.
- Sepsis: Severe infection can cause hypoglycemia.
Management of Hypoglycemia: Immediate and Long-Term Strategies
Managing hypoglycemia involves immediate treatment to raise blood glucose levels and long-term strategies to prevent recurrence.
Immediate Treatment:
- Oral Glucose: For mild hypoglycemia, patients can consume 15-20 grams of fast-acting carbohydrates, such as glucose tablets, fruit juice, or honey.
- Intravenous Glucose: For moderate to severe hypoglycemia, intravenous dextrose is necessary to rapidly elevate blood glucose levels. This is particularly important in unconscious or unresponsive patients.
- Glucagon: Glucagon, a hormone that stimulates the liver to release glucose, can be administered intramuscularly or subcutaneously in cases where intravenous access is difficult or unavailable.
Long-Term Management:
Long-term management focuses on identifying and addressing the underlying cause. This may involve:
- Dietary Modifications: Adjusting carbohydrate intake to prevent significant fluctuations in blood glucose.
- Medication Adjustments: Modifying medications that may be contributing to hypoglycemia.
- Surgical Intervention: Surgical removal of insulinomas or other tumors contributing to hypoglycemia.
- Regular Monitoring: Regular blood glucose monitoring helps to identify and prevent future episodes.
- Patient Education: Educating the patient and their family about the signs, symptoms, and management of hypoglycemia is essential to improve patient outcomes.
Conclusion: A Multifaceted Approach to Hypoglycemia
Assessing a patient with suspected hypoglycemia requires a comprehensive and systematic approach, integrating clinical findings, laboratory investigations, and a careful consideration of the differential diagnosis. Prompt recognition of the signs and symptoms, accurate diagnosis of the underlying cause, and appropriate management are crucial for preventing severe complications and ensuring optimal patient outcomes. Remember, the timely intervention and understanding the nuances of this condition are vital in preventing potentially life-threatening consequences. This requires a team effort involving physicians, nurses, and other healthcare professionals. The multidisciplinary approach ensures accurate assessment, effective treatment and proper patient education to enhance the quality of life for individuals experiencing hypoglycemia.
Latest Posts
Latest Posts
-
One Challenge Faced By The European Union Is The
Mar 20, 2025
-
Letrs Unit 3 Session 2 Check For Understanding
Mar 20, 2025
-
Motivating Operations Can Exert Stimulus Control Over A Behavior By
Mar 20, 2025
-
Managers Can Use An Action Plan To
Mar 20, 2025
-
Which Comment Is About The Diction Of A Story
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Assessment Of A Patient With Hypoglycemia Will Most Likely Reveal . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
