Asthma Is Caused By Which Type Of Response Quizlet
Breaking News Today
Mar 31, 2025 · 6 min read
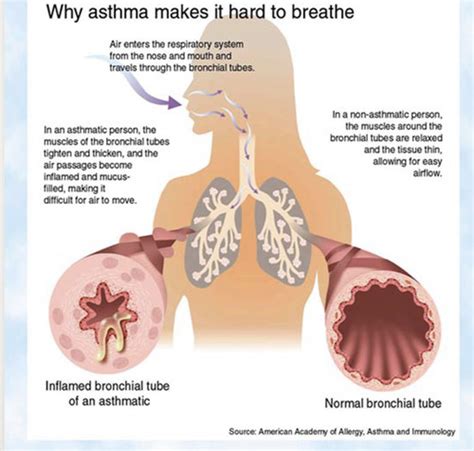
Table of Contents
Asthma: Unpacking the Immunological Response – A Comprehensive Guide
Asthma, a chronic respiratory condition affecting millions worldwide, is characterized by inflammation and narrowing of the airways. Understanding its underlying causes is crucial for effective management and treatment. While environmental triggers play a significant role in asthma attacks, the root cause lies within the body's immune system and its complex response to various stimuli. This article delves deep into the immunological mechanisms behind asthma, clarifying the type of response involved and dispelling common misconceptions.
H2: The Role of the Immune System in Asthma
The immune system, our body's defense against foreign invaders, plays a central role in asthma pathogenesis. Contrary to popular belief, asthma isn't simply a matter of irritated airways; it's a complex interplay of genetic predisposition, environmental factors, and a dysregulated immune response. Specifically, asthma is largely driven by a type 2 immune response.
H3: Type 2 Immune Response: The Key Player
The type 2 immune response involves a specific cascade of immune cells and mediators, including:
-
T helper 2 (Th2) cells: These are the master regulators of the type 2 response. They release cytokines (signaling molecules) that promote inflammation and airway hyperresponsiveness – the hallmarks of asthma. Key cytokines include IL-4, IL-5, and IL-13.
-
IL-4: This cytokine stimulates B cells to produce IgE antibodies.
-
IL-5: This cytokine promotes the growth and activation of eosinophils, a type of white blood cell implicated in asthma inflammation.
-
IL-13: This cytokine contributes to airway mucus production, airway remodeling, and increased airway smooth muscle contractility.
-
Eosinophils: These inflammatory cells infiltrate the airways, releasing substances that damage the airway lining and contribute to airway narrowing. Elevated eosinophil counts in the blood or sputum are often used as diagnostic indicators of asthma severity.
-
Mast cells: These immune cells reside in the airways and release histamine and other inflammatory mediators upon activation, leading to bronchoconstriction (narrowing of the airways) and increased mucus production.
-
IgE antibodies: These antibodies bind to mast cells and basophils, sensitizing them to future exposure to allergens. When re-exposed, this leads to a rapid release of inflammatory mediators, triggering an asthma attack.
H2: The Allergic Pathway and Asthma
Many asthma cases are associated with allergies. The allergic pathway directly involves the type 2 immune response:
-
Initial sensitization: Upon first exposure to an allergen (e.g., pollen, dust mites, pet dander), the immune system identifies it as a foreign substance.
-
Antigen presentation: Dendritic cells, specialized immune cells, capture the allergen and present it to T cells.
-
Th2 cell differentiation: This presentation triggers the differentiation of naive T cells into Th2 cells.
-
IgE production: Th2 cells release IL-4, which stimulates B cells to produce IgE antibodies specific to the allergen.
-
Mast cell sensitization: IgE antibodies bind to mast cells in the airways.
-
Subsequent exposure: Upon subsequent exposure to the same allergen, it binds to the IgE antibodies on mast cells, triggering their degranulation.
-
Inflammatory mediator release: Mast cells release histamine, leukotrienes, and other inflammatory mediators, leading to bronchoconstriction, mucus production, and airway inflammation – the characteristic features of an asthma attack.
H2: Beyond Allergic Asthma: Non-Allergic Asthma and Other Immune Responses
While allergic asthma is common, not all asthma is allergy-driven. Non-allergic asthma, also known as intrinsic asthma, lacks the clear IgE-mediated allergic mechanism. Even in non-allergic asthma, however, a type 2 immune response can still play a significant role, although the triggers might be different. Factors such as viral respiratory infections, air pollution, and exercise can trigger inflammation through different pathways, sometimes involving other immune cells and cytokines.
While type 2 inflammation is dominant in many asthma cases, other immune responses can contribute:
-
Type 1 immune response: This response, primarily involved in immediate hypersensitivity reactions, can play a role in some cases of asthma, particularly those with a strong allergic component.
-
Type 3 immune response: Involving immune complexes, this type of response has been linked to certain forms of asthma but is less prevalent than type 2.
-
Neutrophils: While eosinophils are a hallmark of type 2 inflammation, neutrophils, another type of white blood cell, can also contribute to inflammation in some asthma subtypes, particularly those with more severe disease or those associated with bacterial infections.
H2: Genetic Predisposition and Environmental Factors
The development of asthma is a complex interplay of genetics and environment. Genetic factors influence the individual's susceptibility to developing a type 2 immune response and the severity of the disease. Specific genes involved in immune regulation, airway function, and inflammation have been identified.
Environmental factors, such as exposure to allergens, air pollution, respiratory infections, and smoking, can trigger or exacerbate asthma symptoms. These factors can act as triggers, initiating the inflammatory cascade in susceptible individuals.
H2: Diagnostic Approaches and Assessment of Immune Response
Diagnosing asthma involves a combination of clinical evaluation, spirometry (a lung function test), and potentially other tests to assess the underlying immune response. These tests may include:
- Blood tests: To measure IgE levels and eosinophil counts.
- Sputum analysis: To identify inflammatory cells and mediators in the airway mucus.
- Allergy testing: To identify specific allergens that trigger asthma attacks.
H2: Treatment Strategies Targeting the Immune Response
Treatment for asthma aims to control inflammation and prevent symptoms. This often involves a multi-pronged approach:
-
Inhaled corticosteroids: These medications reduce inflammation in the airways by suppressing the activity of immune cells like eosinophils and mast cells.
-
Bronchodilators: These medications help relax the airway muscles, relieving bronchoconstriction and improving airflow.
-
Biologic therapies: Newer therapies specifically target components of the type 2 immune response. These medications, such as anti-IL-5 or anti-IL-13 antibodies, can significantly reduce inflammation and improve asthma control in patients with severe disease.
-
Allergen avoidance: Avoiding exposure to allergens helps prevent the triggering of an immune response and subsequent asthma attacks.
H2: Conclusion: Asthma is Primarily a Type 2 Immune Response
While the exact mechanisms are complex and still under investigation, the overwhelming evidence points to a type 2 immune response as the central player in the pathogenesis of asthma, particularly in allergic asthma. Understanding this crucial aspect is fundamental for developing effective diagnostic tools and therapies that target the root cause of the disease and improve the lives of those living with asthma. Further research continues to unravel the intricacies of this complex condition and refine treatment approaches to better manage the disease burden for millions of affected individuals globally. This understanding emphasizes the importance of personalized medicine approaches, taking into account the individual's genetic predisposition and specific immune profile to tailor treatment strategies for optimal outcomes. The ongoing exploration of immunomodulatory therapies and precise allergen identification promises a future of more effective and personalized asthma management.
Latest Posts
Latest Posts
-
In The Hospitality Industry The Concept Of Perishability Means
Apr 02, 2025
-
Where Do Broadside Collisions Most Commonly Occur
Apr 02, 2025
-
El Aprendizaje Servicio Consiste En Ir A Cursos De Verano
Apr 02, 2025
-
Completa Las Oraciones Usando El Preterito De Ser O Ir
Apr 02, 2025
-
Unit 7 Progress Check Mcq Ap World
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Asthma Is Caused By Which Type Of Response Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
