Common Causes Of Syncope In Older Patients Quizlet
Breaking News Today
Mar 31, 2025 · 6 min read
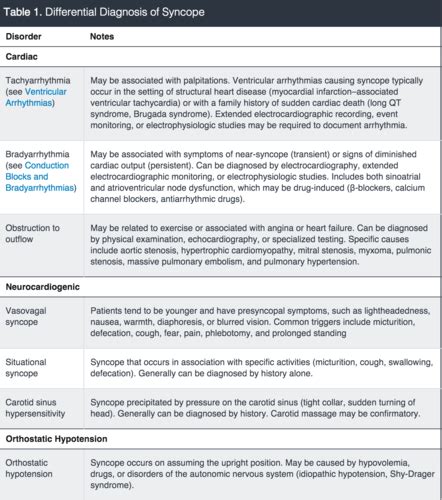
Table of Contents
Common Causes of Syncope in Older Patients: A Comprehensive Guide
Syncope, or fainting, is a common condition characterized by a temporary loss of consciousness followed by spontaneous recovery. While it can affect individuals of all ages, older adults are particularly susceptible due to age-related physiological changes and the increased prevalence of underlying medical conditions. Understanding the common causes of syncope in older patients is crucial for accurate diagnosis and appropriate management. This comprehensive guide will delve into the various etiologies, highlighting key differences and risk factors, and ultimately aiding in the differential diagnosis.
Cardiovascular Causes: The Major Players
Cardiovascular diseases represent a significant proportion of syncope cases in the elderly population. These conditions often disrupt the normal blood flow to the brain, leading to a transient loss of consciousness.
1. Orthostatic Hypotension:
Orthostatic hypotension, a sudden drop in blood pressure upon standing, is a frequent cause of syncope in older adults. The autonomic nervous system's ability to regulate blood pressure efficiently declines with age, making individuals more prone to this condition.
-
Mechanism: The baroreceptor reflex, responsible for maintaining blood pressure, becomes less sensitive. This results in inadequate vasoconstriction and reduced cardiac output when changing from a lying or sitting position to standing, leading to cerebral hypoperfusion and syncope.
-
Risk Factors: Dehydration, medications (e.g., diuretics, antihypertensives), autonomic neuropathy (diabetes, Parkinson's disease), and prolonged bed rest all contribute to orthostatic hypotension.
-
Clinical Presentation: Dizziness, lightheadedness, blurred vision, and weakness preceding the syncopal episode are common symptoms.
2. Cardiac Arrhythmias:
Irregular heartbeats, or arrhythmias, significantly increase the risk of syncope, especially in older patients. These arrhythmias can disrupt the normal rhythm and reduce cardiac output, resulting in insufficient blood flow to the brain.
-
Types: Bradycardia (slow heart rate), tachycardia (rapid heart rate), and various types of heart blocks are common culprits. Atrial fibrillation, a common arrhythmia in the elderly, can lead to syncope through mechanisms like reduced stroke volume and the formation of thrombi.
-
Risk Factors: Underlying heart disease (coronary artery disease, valvular heart disease), electrolyte imbalances, and medications can trigger or exacerbate arrhythmias.
-
Clinical Presentation: Syncope can be sudden and without warning, often accompanied by palpitations or chest pain.
3. Valvular Heart Disease:
Aortic stenosis, a narrowing of the aortic valve, is a significant cause of syncope in older adults. The reduced blood flow from the left ventricle into the aorta limits the amount of blood reaching the brain, particularly during periods of increased demand.
-
Mechanism: The narrowed aortic valve obstructs blood flow, resulting in decreased cardiac output and cerebral hypoperfusion. Syncope often occurs during exertion, reflecting the increased demand on the heart.
-
Risk Factors: Age-related degenerative changes in the aortic valve, rheumatic heart disease.
-
Clinical Presentation: Syncope is usually associated with exertion, but it can also occur at rest in severe cases. Other symptoms include angina (chest pain) and shortness of breath.
Neurological Causes: A Less Frequent but Important Consideration
While cardiovascular causes dominate, neurological conditions can also contribute to syncope in older individuals.
1. Vasovagal Syncope (Neurocardiogenic Syncope):
Vasovagal syncope, the most common type of reflex syncope, results from an overreaction of the autonomic nervous system to triggers like stress, pain, or prolonged standing. It often manifests as a prodrome of nausea, pallor, sweating, and a feeling of warmth.
-
Mechanism: Activation of vagal nerves slows the heart rate, causing bradycardia. Simultaneously, vasodilation reduces blood pressure, leading to cerebral hypoperfusion and syncope.
-
Risk Factors: Dehydration, prolonged standing, emotional stress, and certain medical conditions.
-
Clinical Presentation: The prodromal symptoms are characteristic, followed by a gradual loss of consciousness and spontaneous recovery.
2. Carotid Sinus Syncope:
Carotid sinus syncope results from excessive sensitivity of the carotid sinus baroreceptors, located in the carotid arteries. Pressure on these receptors can trigger a reflex bradycardia and vasodilation, leading to syncope.
-
Mechanism: Gentle pressure on the carotid sinus, often during turning the head, shaving, or tight collar, stimulates the baroreceptors, initiating a reflex response resulting in syncope.
-
Risk Factors: Aging, atherosclerosis, and certain medications.
-
Clinical Presentation: Syncope often occurs during specific head movements or neck manipulation.
3. Stroke (Transient Ischemic Attack or TIA):
While less frequently presenting as isolated syncope, stroke or a TIA can cause a sudden loss of consciousness, although often with other neurological symptoms.
-
Mechanism: Disruption of blood flow to the brain due to a blood clot or hemorrhage causes neurological dysfunction, possibly including loss of consciousness.
-
Risk Factors: Hypertension, atherosclerosis, atrial fibrillation.
-
Clinical Presentation: Often accompanied by other neurological deficits such as weakness, speech disturbances, or visual changes. This differentiates it from simple syncope.
Other Less Common Causes: Exploring the Possibilities
Several other less frequent causes of syncope in older patients should be considered, particularly when the more common etiologies have been ruled out.
1. Metabolic Disorders:
Hypoglycemia (low blood sugar), electrolyte imbalances (hypokalemia, hyponatremia), and severe dehydration can all lead to syncope due to insufficient blood flow to the brain.
2. Medication Side Effects:
Various medications, including antihypertensives, diuretics, and certain antidepressants, can cause orthostatic hypotension or other cardiovascular effects that contribute to syncope.
3. Pulmonary Embolism:
A pulmonary embolism, a blood clot in the lungs, can cause sudden shortness of breath and even syncope due to reduced oxygen supply to the brain.
4. Cardiac Tumors:
Rarely, cardiac tumors can obstruct blood flow or interfere with the heart's electrical conduction system, leading to syncope.
5. Aortic Dissection:
A tear in the aorta can cause severe chest pain and syncope due to impaired blood flow. This is a life-threatening condition requiring immediate medical attention.
Diagnostic Approach: Unraveling the Mystery
Diagnosing the cause of syncope in older patients requires a thorough evaluation that includes a detailed medical history, physical examination, and appropriate investigations.
-
Detailed History: This is crucial and includes questioning about the circumstances of the syncope, associated symptoms (prodrome, palpitations, chest pain), medications, medical history, and family history of cardiovascular disease.
-
Physical Examination: This focuses on cardiovascular and neurological assessments, including blood pressure measurement in different positions, heart auscultation, and neurological examination.
-
Investigations: Electrocardiography (ECG) is essential for detecting arrhythmias. Echocardiography can evaluate cardiac structure and function. Tilt-table testing can assess for orthostatic hypotension and vasovagal syncope. Carotid sinus massage may be performed in selected cases. Further investigations like cardiac catheterization or neurological imaging may be needed depending on the clinical suspicion.
Management Strategies: Tailoring Treatment to the Cause
The management of syncope depends entirely on the underlying cause. Treatment aims to address the underlying condition and prevent further episodes.
-
Cardiovascular Causes: Treatment for cardiac arrhythmias may involve medication, pacemaker implantation, or catheter ablation. For valvular heart disease, valve repair or replacement surgery may be necessary. Orthostatic hypotension may be managed by increasing fluid intake, adjusting medications, and implementing lifestyle modifications like compression stockings.
-
Neurological Causes: Treatment for vasovagal syncope often focuses on lifestyle modifications like avoiding triggers and increasing fluid and salt intake. Carotid sinus syncope may require medication or pacemaker implantation.
-
Other Causes: Management strategies are tailored to the specific underlying condition, such as managing diabetes for diabetic neuropathy or treating hypoglycemia.
Conclusion: A Multifaceted Approach
Syncope in older patients is a complex clinical problem requiring a thorough evaluation and a multifaceted approach to diagnosis and management. The focus should always be on identifying the underlying cause, which necessitates a comprehensive history, meticulous physical examination, and appropriate investigations. By accurately identifying the cause and implementing tailored management strategies, the risk of recurrent syncope can be significantly reduced, thus improving the overall health and well-being of older patients. This detailed understanding, coupled with a proactive approach to diagnosis, is crucial to ensuring positive patient outcomes and preventing potentially life-threatening complications. Remember, always consult a medical professional for any concerns regarding syncope or other health issues.
Latest Posts
Latest Posts
-
A Monopolist Does Not Have A Supply Curve Because
Apr 01, 2025
-
The Practice Manager Or A Designee May Be Responsible For
Apr 01, 2025
-
An Organizational Psychologist Studies Such Topics As
Apr 01, 2025
-
Cuando Me Siento Mal El Doctor Me
Apr 01, 2025
-
Which Of The Following Is True About Depression
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Common Causes Of Syncope In Older Patients Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
