Comprehensive Physical Assessment Of A Child Posttest
Breaking News Today
Mar 13, 2025 · 6 min read
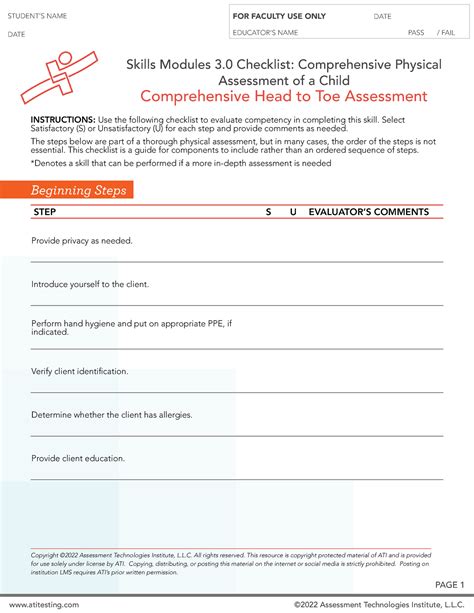
Table of Contents
Comprehensive Physical Assessment of a Child: Post-Test Review
This post-test review delves into the crucial aspects of performing a comprehensive physical assessment on a child. We'll explore the key components, techniques, and considerations necessary for accurate and thorough evaluations. This in-depth guide is designed to enhance your understanding and skills in pediatric physical assessment. It's aimed at students, healthcare professionals, and anyone seeking to improve their proficiency in this vital area.
Understanding the Importance of Pediatric Physical Assessment
A comprehensive physical assessment is fundamental to pediatric healthcare. It forms the cornerstone of diagnosis, treatment planning, and ongoing monitoring of a child's health. Unlike adult assessments, pediatric assessments require a nuanced approach, considering the developmental stage, communication abilities, and unique physiological characteristics of the child. Early detection of abnormalities through meticulous assessment is critical for optimal outcomes and preventing long-term complications.
Key Components of a Comprehensive Pediatric Physical Assessment
A complete physical assessment of a child typically encompasses several key areas. These should be approached systematically and age-appropriately.
1. Preparation and Building Rapport
Before commencing the assessment, establishing a comfortable and trusting environment is paramount. This involves:
- Introducing yourself: Speak clearly and calmly, explaining the procedure in age-appropriate terms.
- Gaining parental consent: Ensure you have appropriate consent before starting the assessment.
- Creating a safe and comfortable space: Use toys, games, or distraction techniques to ease anxiety in young children.
- Observing the child's behavior: Note their alertness, responsiveness, and overall demeanor. This provides valuable insights even before the physical examination begins.
2. General Appearance and Vital Signs
This initial observation forms the foundation of the assessment:
- General Appearance: Assess the child's overall state of health, noting any signs of distress, pallor, cyanosis, or unusual behavior. Observe their posture, level of activity, and nutritional status.
- Weight and Height: Accurate measurements are crucial for monitoring growth and development, detecting potential nutritional deficiencies or growth disorders. Use appropriate age-specific growth charts for comparison.
- Vital Signs: Accurately measure temperature, pulse, respiratory rate, and blood pressure, adjusting techniques as needed for age and cooperation level. Understand the normal ranges for different age groups and identify any significant deviations.
- Pain Assessment: Utilize age-appropriate pain scales to assess pain levels and manage discomfort effectively.
3. Skin Assessment
A thorough skin assessment is vital:
- Inspection: Examine the skin for color, texture, turgor, lesions (rashes, bruises, birthmarks), and any signs of infection or inflammation. Pay attention to skin temperature and moisture.
- Palpation: Assess skin turgor by gently pinching the skin. Decreased turgor may indicate dehydration. Note any areas of tenderness, warmth, or induration.
4. Head and Neck Assessment
This section focuses on various aspects of the head and neck:
- Head: Assess head size and shape (microcephaly, macrocephaly), fontanelles (in infants), scalp for lesions or abnormalities, and facial symmetry.
- Eyes: Examine the eyes for visual acuity, pupillary response, conjunctiva, sclera, and any signs of infection or abnormalities.
- Ears: Assess ear alignment, external canal, and tympanic membrane (using otoscope). Test hearing acuity using age-appropriate techniques.
- Nose: Inspect the nose for patency, discharge, and any signs of nasal flaring or congestion.
- Mouth and Throat: Examine the oral cavity for dental hygiene, gum health, tongue, tonsils, and palate. Look for lesions, ulcers, or signs of infection.
- Neck: Palpate the neck for lymph nodes (size, tenderness, mobility), trachea position, and thyroid gland. Assess neck range of motion.
5. Respiratory Assessment
Thorough respiratory assessment is critical, especially in children prone to respiratory illnesses:
- Observation: Observe the respiratory rate, rhythm, depth, and effort. Note any signs of respiratory distress, such as nasal flaring, retractions, grunting, or wheezing.
- Auscultation: Auscultate the lungs bilaterally, listening for breath sounds (normal, diminished, adventitious). Identify any crackles, wheezes, or rhonchi.
6. Cardiovascular Assessment
This area focuses on the heart and circulatory system:
- Inspection: Observe for any visible pulsations, cyanosis, or edema.
- Palpation: Palpate the apical impulse and assess for thrills or heaves.
- Auscultation: Auscultate the heart sounds in all five auscultatory areas, noting rate, rhythm, and any abnormal heart sounds (murmurs, clicks, rubs).
7. Gastrointestinal Assessment
This involves assessing the abdomen and digestive system:
- Inspection: Observe the abdomen for contour, distension, scars, and visible peristalsis.
- Auscultation: Auscultate bowel sounds in all four quadrants. Note frequency and character of bowel sounds.
- Palpation: Gently palpate the abdomen for tenderness, masses, or organomegaly. Note any guarding or rigidity.
8. Genitourinary Assessment
This section requires sensitivity and age-appropriate techniques:
- Inspection: Inspect the external genitalia for hygiene, abnormalities, or signs of infection.
- Palpation: Palpate the kidneys and bladder (if indicated and age-appropriate).
9. Musculoskeletal Assessment
Assessing the musculoskeletal system includes:
- Inspection: Observe posture, gait, and range of motion of all extremities. Note any deformities, asymmetry, or swelling.
- Palpation: Palpate bones, joints, and muscles for tenderness, swelling, or crepitus. Assess muscle strength and tone.
10. Neurological Assessment
This critical assessment encompasses several aspects:
- Level of Consciousness: Assess the child's alertness, responsiveness, and orientation.
- Cranial Nerves: Assess cranial nerve function using age-appropriate methods.
- Motor Function: Assess gross and fine motor skills, coordination, strength, and reflexes.
- Sensory Function: Test sensation using appropriate stimuli.
11. Documentation
Meticulous documentation is essential. Record all findings clearly and concisely, including:
- Chief Complaint: The reason for the visit.
- History: Relevant medical history, including past illnesses, surgeries, allergies, and medications.
- Physical Examination: Detailed description of all findings, including vital signs, general appearance, and findings from each system review.
- Assessment: Interpretation of findings and potential diagnoses.
- Plan: Treatment plan, including medications, referrals, and follow-up appointments.
Age-Specific Considerations in Pediatric Physical Assessment
The approach to a physical assessment varies significantly depending on the child's age:
- Infants (0-12 months): Assessments focus on reflexes, growth parameters, feeding habits, and developmental milestones. Utilize calming techniques to minimize stress.
- Toddlers (1-3 years): Engage the child with toys and games to enhance cooperation. Quick and efficient assessments are key.
- Preschoolers (3-5 years): Allow the child to participate in the assessment to build trust and cooperation. Use simple language and explanations.
- School-Aged Children (6-12 years): Explain the procedure clearly and allow them to ask questions. Incorporate privacy and respect.
- Adolescents (13-18 years): Maintain confidentiality and respect their privacy. Address specific concerns related to puberty and adolescent health.
Challenges and Ethical Considerations
Performing a comprehensive pediatric assessment can present various challenges:
- Limited Communication: Young children may have difficulty communicating their symptoms or concerns.
- Fear and Anxiety: Children may be apprehensive about the examination.
- Parental Involvement: Balancing parental involvement with the need for a thorough assessment can be challenging.
- Ethical Considerations: Maintaining confidentiality and respecting the child's autonomy are paramount.
Conclusion
Mastering the art of comprehensive pediatric physical assessment is a continuous learning process. By understanding the key components, employing appropriate techniques, and considering age-specific needs, healthcare providers can ensure accurate diagnoses, effective treatment planning, and optimal outcomes for children. Continuous professional development and adherence to ethical guidelines are essential for providing high-quality pediatric care. Remember, a thorough and sensitive approach builds trust and facilitates accurate assessment, contributing to the overall well-being of the child.
Latest Posts
Latest Posts
-
Should You Always Drive Slower Than Other Traffic
Mar 13, 2025
-
What Are Some Of The Resources Available For Online Learning
Mar 13, 2025
-
Most Transportation Management Systems Optimize Mode Selection
Mar 13, 2025
-
Becoming A Leader Consists Of What Total Number Of Paths
Mar 13, 2025
-
Student Exploration Coral Reefs 1 Abiotic Factors
Mar 13, 2025
Related Post
Thank you for visiting our website which covers about Comprehensive Physical Assessment Of A Child Posttest . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
