Define Medical Necessity As It Applies To Procedural Coding
Breaking News Today
Apr 07, 2025 · 6 min read
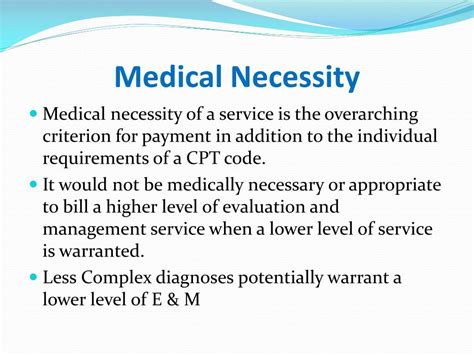
Table of Contents
Defining Medical Necessity in Procedural Coding: A Comprehensive Guide
Medical necessity is a cornerstone of accurate procedural coding and reimbursement in healthcare. Understanding its nuances is crucial for medical coders, billers, physicians, and healthcare administrators to ensure compliance, efficient billing practices, and ultimately, patient care. This comprehensive guide delves into the definition of medical necessity, its implications for procedural coding, and the challenges involved in its determination.
What is Medical Necessity?
Medical necessity, in the context of procedural coding, signifies that a healthcare service or procedure is reasonable and necessary for the diagnosis or treatment of an illness, injury, condition, disease, or its symptoms. It's not simply about what a patient wants, but what they need based on sound medical judgment. This judgment is rooted in evidence-based medicine, accepted medical standards, and the physician's professional expertise. A service or procedure lacking medical necessity is considered unnecessary and may not be reimbursed by insurance payers.
Key elements of medical necessity include:
- Reasonable: The service or procedure must be in line with commonly accepted medical practices within the relevant specialty. This implies using evidence-based guidelines, adhering to clinical pathways, and considering the patient's specific circumstances.
- Necessary: The service or procedure must be essential for the effective diagnosis or treatment of the patient's condition. This means there are no less invasive or costly alternatives that would achieve the same or better outcome.
- Appropriate: The service or procedure must be tailored to the individual patient's needs and circumstances. This involves considering factors like age, medical history, and overall health status.
The Role of Medical Necessity in Procedural Coding
Accurate procedural coding hinges on establishing medical necessity. When a physician orders a procedure, the coder must ensure the procedure code accurately reflects the service provided and that the service was medically necessary. Incorrect coding due to a lack of medical necessity can lead to:
- Reimbursement denials: Insurance companies rigorously review claims for medical necessity. Claims lacking sufficient documentation supporting medical necessity are often denied.
- Audits and penalties: Healthcare providers are subject to audits by payers and government agencies. Consistent lack of medical necessity documentation can result in significant financial penalties and reputational damage.
- Legal ramifications: In extreme cases, billing for non-medically necessary procedures can lead to legal action and accusations of fraud.
Documentation is Key: Supporting Medical Necessity
The most critical aspect of demonstrating medical necessity is thorough and comprehensive documentation. This documentation should clearly link the diagnosis to the procedure performed, demonstrating the direct relationship between the two. The documentation should include:
- Detailed history and physical examination: This outlines the patient's symptoms, medical history, relevant findings from the physical examination, and any other pertinent clinical information. It establishes the clinical basis for the need for the procedure.
- Diagnostic testing results: Lab reports, imaging studies (X-rays, CT scans, MRIs), and other diagnostic tests provide objective evidence supporting the diagnosis and the necessity of the procedure.
- Treatment plan: The documentation should articulate the physician's rationale for selecting the specific procedure, justifying its choice over other possible interventions. It should also explain the expected benefits and potential risks of the procedure.
- Progress notes: These should document the patient's response to the treatment, any changes in their condition, and the overall effectiveness of the procedure. This ensures that the procedure was indeed necessary and produced the intended outcome.
- Consultation reports: If consultations with specialists were involved, their reports should be included to provide additional support for the medical necessity of the procedure.
Specific examples of documentation requirements depending on the procedure:
- Surgery: Detailed operative notes, including indications, operative findings, and postoperative course.
- Imaging: Detailed radiology reports correlating findings to clinical presentation.
- Laboratory tests: Comprehensive lab reports detailing results and their clinical significance.
- Physical Therapy: Documentation of the patient's functional limitations, treatment plan, and progress notes demonstrating improvement.
Challenges in Determining Medical Necessity
Determining medical necessity is not always straightforward. Several factors can complicate the process:
- Subjectivity: Medical judgment often involves subjective elements. Different physicians may have slightly different approaches to diagnosis and treatment, which can lead to varying opinions on medical necessity.
- Lack of clear guidelines: While guidelines exist, they are not always comprehensive or specific enough to cover every clinical scenario. Ambiguity can create challenges in determining medical necessity.
- Evolving medical knowledge: Medical knowledge is constantly evolving. New treatments and technologies emerge, requiring ongoing updates to guidelines and criteria for medical necessity.
- Payer variations: Different payers (insurance companies, Medicare, Medicaid) may have slightly varying criteria for determining medical necessity. This necessitates careful review of each payer's specific policies and guidelines.
- Pressure to perform unnecessary procedures: In some cases, there might be pressure to perform procedures that are not medically necessary, driven by financial incentives or other factors. This underlines the importance of ethical considerations in medical decision-making.
Navigating Medical Necessity Disputes
Even with meticulous documentation, disputes regarding medical necessity can arise. When a claim is denied due to a question of medical necessity, several steps can be taken:
- Review the denial letter: Carefully examine the reason provided by the payer for the denial. This will pinpoint the areas where the documentation may be lacking.
- Appeal the decision: Most payers have an appeals process. Gather additional supporting documentation and submit a well-reasoned appeal.
- Consult with a medical coding expert: A qualified expert can review the documentation and identify any deficiencies or provide guidance on strengthening the appeal.
- Engage in peer-to-peer review: This involves a discussion between the treating physician and a physician employed by the payer to clarify any uncertainties regarding the medical necessity of the procedure.
The Future of Medical Necessity
The determination of medical necessity is likely to become even more complex in the future due to advancements in healthcare technology and data analytics. The increasing use of electronic health records (EHRs) and big data offers opportunities to improve the accuracy and efficiency of medical necessity determination. However, challenges related to data privacy, security, and interoperability need to be addressed.
Conclusion
Medical necessity is not merely a billing requirement; it is a critical element of ethical and responsible healthcare delivery. Understanding its complexities, meticulously documenting its justification, and navigating potential disputes are crucial for ensuring that patients receive appropriate care and that healthcare providers are fairly compensated for their services. By diligently following these guidelines, healthcare providers can uphold their commitment to high-quality, necessary care and navigate the intricate world of procedural coding and reimbursement with greater confidence and success. Maintaining accurate records, staying updated on guidelines and regulations, and building strong relationships with payers are all essential for successful navigation of the medical necessity landscape. This meticulous approach is paramount in fostering trust and promoting a sustainable healthcare system.
Latest Posts
Latest Posts
-
Their Eyes Were Watching God Chapter Summary
Apr 07, 2025
-
Prokaryotes Can Store Excess Proteins In Cellular Aggregations Called Blank
Apr 07, 2025
-
Which Of These Rhetorical Devices Is Most Clearly Used Here
Apr 07, 2025
-
Hilda Just Got Her First Sales Position
Apr 07, 2025
-
Susana Has Decided To Write About Her Friend
Apr 07, 2025
Related Post
Thank you for visiting our website which covers about Define Medical Necessity As It Applies To Procedural Coding . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.