Echelon Prevention Of Medical Errors Test Answers
Breaking News Today
Apr 01, 2025 · 6 min read
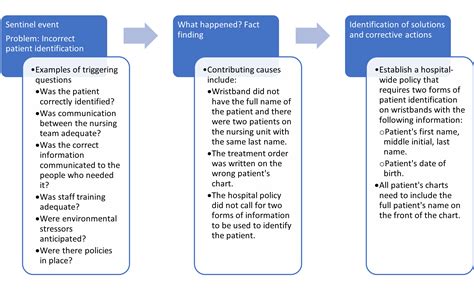
Table of Contents
Echelon Prevention of Medical Errors: Test Answers and a Deeper Dive into Patient Safety
Medical errors remain a significant concern in healthcare, impacting patient safety and outcomes globally. Implementing robust prevention strategies is paramount. This article delves into the concept of "echelon prevention," a multi-layered approach to minimizing errors, providing insights into potential test answers and a broader understanding of patient safety initiatives. While specific "test answers" are context-dependent (depending on the specific test and curriculum), we'll explore the core principles underlying effective error prevention.
Understanding Echelon Prevention
Echelon prevention, in the context of medical errors, refers to a layered approach to safety. Instead of relying on a single preventative measure, it employs multiple safeguards at different levels, creating a "defense in depth" strategy. If one layer fails, others are in place to catch the error before it reaches the patient. Think of it like a castle with multiple walls and defenses—a breach of one doesn't necessarily compromise the entire structure.
This multi-layered approach addresses errors at various points in the healthcare process, encompassing:
- Individual practitioner level: This focuses on the skills, knowledge, and behaviors of individual healthcare providers.
- Team level: This focuses on improving communication, collaboration, and teamwork among healthcare professionals.
- Organizational level: This involves creating a culture of safety within the healthcare organization, implementing robust systems and processes, and ensuring adequate resources are available.
- System level: This looks at broader societal factors like policy, regulation and technology.
Core Principles of Echelon Prevention: Potential Test Answer Themes
Understanding the underlying principles is key to answering questions about echelon prevention. Here are some core concepts that are frequently tested:
1. Human Factors Engineering
What it is: This addresses the limitations of human capabilities and designs systems and processes to minimize error. It considers factors like fatigue, stress, cognitive biases, and workload.
Potential Test Questions & Answers:
-
Q: How does human factors engineering contribute to echelon prevention?
-
A: Human factors engineering minimizes error by designing systems that account for human limitations. This could involve simplifying complex procedures, using clear and concise communication protocols, and designing user-friendly interfaces for medical equipment. It contributes to all echelons, from designing error-proof systems at the organizational level to educating individuals on best practices at the practitioner level.
-
Q: Give an example of human factors engineering in a clinical setting.
-
A: Using barcoding systems to verify medication administration before dispensing, designing medication carts with clear labeling and logical organization, standardizing equipment placement to minimize searching and reduce distractions. These improve processes at all levels preventing errors at individual and team levels.
2. Standardization and Protocols
What it is: Standardized procedures and protocols reduce variability and provide clear guidelines for healthcare providers to follow. This eliminates ambiguity and minimizes the potential for individual errors.
Potential Test Questions & Answers:
-
Q: Why are standardized protocols crucial for echelon prevention?
-
A: Standardized protocols reduce variations in practice, creating consistency and reducing the likelihood of errors. By clearly defining steps and procedures, they leave less room for individual interpretation and potential mistakes. This acts as a primary preventative layer across multiple echelons.
-
Q: Explain the benefits of using standardized checklists in surgery.
-
A: Surgical checklists improve team communication, reduce missed steps, and improve patient safety. They act as a crucial layer at the team level, reducing the likelihood of errors stemming from poor communication or missed steps during complex procedures. They support the individual practitioner as well by reducing their cognitive load during stressful procedures.
3. Teamwork and Communication
What it is: Effective teamwork and communication are essential for preventing medical errors. Clear communication channels, shared situational awareness, and a collaborative approach reduce the risk of miscommunication and misunderstandings.
Potential Test Questions & Answers:
-
Q: How does effective team communication contribute to echelon prevention?
-
A: Effective communication reduces the potential for misinterpretations and missed information. Using structured communication techniques, such as SBAR (Situation, Background, Assessment, Recommendation), ensures clear and concise information exchange. This is pivotal in team-based care, preventing misunderstandings that could lead to errors.
-
Q: Describe the role of situation awareness in preventing medical errors.
-
A: Situation awareness refers to a healthcare provider's understanding of the patient's condition, the treatment plan, and the current status of the situation. This is fundamental across all levels, facilitating effective decision making and reducing the risk of errors. Shared situation awareness across the team improves coordination and prevents unintended consequences from individual actions.
4. Error Reporting and Analysis
What it is: A culture of safety encourages reporting near misses and errors without blame. Analyzing these incidents allows healthcare organizations to identify systemic weaknesses and implement improvements.
Potential Test Questions & Answers:
-
Q: Why is error reporting crucial for improving patient safety?
-
A: Error reporting provides valuable data for identifying trends, systemic weaknesses, and areas for improvement in patient safety. A non-punitive culture encourages reporting, revealing patterns that might otherwise go unnoticed. This analysis informs changes at all organizational levels, improving systems and processes for enhanced safety.
-
Q: How can root cause analysis help improve patient safety?
-
A: Root cause analysis goes beyond identifying the immediate cause of an error to uncover underlying factors that contributed to the event. This allows organizations to implement targeted interventions to address the root causes, preventing similar errors in the future, strengthening preventative measures in every echelon.
5. Technology and Automation
What it is: Utilizing technology and automation can reduce manual processes, improve data accuracy, and create safeguards against human error.
Potential Test Questions & Answers:
-
Q: How can technology contribute to echelon prevention of medical errors?
-
A: Technology can automate tasks prone to human error, such as medication dispensing or diagnostic testing. Electronic health records improve information accessibility and reduce transcription errors. Clinical decision support systems provide alerts and reminders, improving patient safety.
-
Q: Discuss the benefits and limitations of using electronic health records (EHRs) in preventing errors.
-
A: EHRs improve data accessibility and reduce transcription errors. However, they can also contribute to alert fatigue if not implemented effectively, creating challenges for the individual user.
Beyond the Test: A Broader Perspective on Patient Safety
While understanding the core principles and potential test questions is crucial, a deeper understanding of patient safety initiatives goes beyond exam preparation. It requires a commitment to a culture of safety that permeates every aspect of the healthcare system.
Key aspects to consider:
- Just Culture: A just culture fosters open communication and reporting of errors without fear of blame. It focuses on learning from mistakes rather than assigning blame.
- High-Reliability Organizations (HROs): Studying HROs, like aviation and nuclear power, reveals best practices for preventing errors in high-stakes environments. These principles can be adapted to healthcare settings.
- Continuous Quality Improvement (CQI): CQI involves ongoing monitoring, evaluation, and improvement of healthcare processes. Data analysis is key to identifying areas for improvement.
- Patient Empowerment: Involving patients in their own care enhances safety by fostering better communication and shared decision-making.
Conclusion: Building a Safer Healthcare System
Echelon prevention of medical errors is not just about passing a test; it's about building a safer and more reliable healthcare system. By understanding and implementing the principles discussed here—human factors engineering, standardization, teamwork, error reporting, and technology—we can significantly reduce medical errors and improve patient outcomes. It’s a continuous process of learning, adaptation, and improvement, requiring a collective commitment to patient safety across all levels of the healthcare system. The ultimate goal is not merely to answer test questions correctly, but to contribute to a future where preventable medical errors are minimized, and patient safety is paramount.
Latest Posts
Latest Posts
-
Decidimos Venir A Este Restaurante Porque Mi Jefe
Apr 02, 2025
-
Skills Module 3 0 Intravenous Medication Administration Posttest
Apr 02, 2025
-
America The Story Of Us Episode 9 Bust
Apr 02, 2025
-
How Did Kuba Artists Decorate Their Ngady Amawaash Masks
Apr 02, 2025
-
A Research Study Using Naturalistic Observation Entails
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Echelon Prevention Of Medical Errors Test Answers . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
