Functions Of The Liver Include Quizlet Emt
Breaking News Today
Mar 31, 2025 · 6 min read
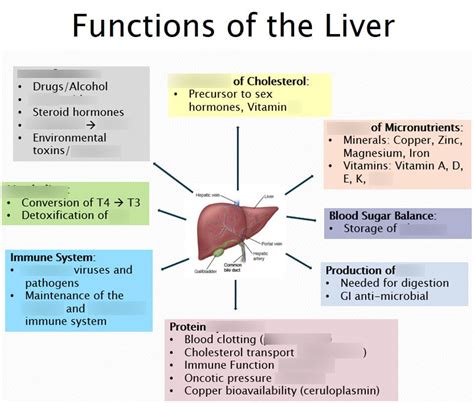
Table of Contents
The Liver: A Vital Organ and Its Functions – An EMT Perspective
The liver, often overlooked in everyday conversation, is a powerhouse organ crucial for survival. Understanding its multifaceted functions is paramount for Emergency Medical Technicians (EMTs), as liver dysfunction significantly impacts a patient's overall health and can present in various ways during emergencies. This comprehensive guide delves into the key functions of the liver, highlighting their significance in emergency medical situations and providing a foundation for accurate assessment and treatment. We'll explore the liver's role in metabolism, detoxification, and synthesis, emphasizing the clinical implications of its malfunction.
1. Metabolism: The Liver's Central Role
The liver acts as the body's central metabolic hub, playing a vital role in processing carbohydrates, proteins, and fats. Let's break down each metabolic pathway:
1.1 Carbohydrate Metabolism:
- Glycogenesis: The liver stores excess glucose as glycogen, a readily available energy source. This process is crucial for maintaining blood glucose levels between meals. Impaired glycogenesis can lead to hypoglycemia, a potentially life-threatening condition requiring immediate medical intervention.
- Glycogenolysis: When blood glucose levels drop, the liver breaks down glycogen back into glucose through glycogenolysis, ensuring a constant supply of energy for the body. Disruptions in this process can also contribute to hypoglycemia.
- Gluconeogenesis: If glycogen stores are depleted, the liver can synthesize glucose from non-carbohydrate sources like amino acids and glycerol (from fats). This process is essential during prolonged fasting or starvation. Failure of gluconeogenesis can severely compromise the body's energy supply.
1.2 Protein Metabolism:
- Amino Acid Metabolism: The liver plays a critical role in processing amino acids, breaking them down, converting them into energy or other compounds, and synthesizing essential proteins.
- Deamination: The liver removes the amino group (NH2) from amino acids, converting them into ammonia (NH3). Ammonia is highly toxic, so the liver swiftly converts it into urea, a less toxic compound excreted by the kidneys. Impaired liver function can lead to an accumulation of ammonia in the blood (hyperammonemia), causing neurological symptoms like confusion, lethargy, and even coma.
- Protein Synthesis: The liver synthesizes many essential proteins, including albumin, clotting factors, and transport proteins. Albumin, a major blood protein, maintains blood osmotic pressure. Deficiencies can cause edema (fluid retention). Liver failure compromises the synthesis of clotting factors, increasing the risk of bleeding.
1.3 Lipid Metabolism:
- Lipogenesis: The liver synthesizes fatty acids and triglycerides from excess carbohydrates and proteins. This process contributes to energy storage and the production of lipoproteins that transport fats in the bloodstream.
- Lipolysis: The liver breaks down triglycerides into fatty acids and glycerol. This process provides energy when glucose levels are low.
- Cholesterol Metabolism: The liver plays a significant role in cholesterol synthesis and excretion. Disrupted cholesterol metabolism can contribute to the buildup of cholesterol in the blood, leading to atherosclerosis and cardiovascular disease.
2. Detoxification: The Liver's Protective Role
The liver acts as a powerful detoxifying organ, neutralizing and eliminating various harmful substances. This process involves:
- Drug Metabolism: The liver metabolizes many drugs, converting them into less active or inactive forms that can be excreted. This process can significantly affect drug efficacy and duration of action. Liver dysfunction can lead to drug accumulation, resulting in toxicity. EMTs need to be aware of this interaction when dealing with patients on multiple medications.
- Alcohol Metabolism: The liver metabolizes alcohol, converting it into acetaldehyde, a toxic compound, then further into acetate. Chronic alcohol abuse overwhelms the liver's capacity, leading to fatty liver disease, alcoholic hepatitis, and cirrhosis.
- Bilirubin Metabolism: Bilirubin, a breakdown product of heme (a component of hemoglobin), is transported to the liver where it is conjugated (made water-soluble) and excreted in bile. Impaired bilirubin metabolism leads to jaundice (yellowing of the skin and eyes). Jaundice is a critical sign of liver dysfunction and requires immediate attention.
- Toxins and Waste Products: The liver removes various toxins and waste products from the blood, including ammonia, hormones, and other harmful chemicals. Liver damage can compromise this detoxifying function, leading to a buildup of toxins in the body.
3. Synthesis and Secretion: Essential Liver Functions
The liver synthesizes and secretes several essential substances, including:
- Bile: Bile is essential for the digestion and absorption of fats. It is produced by the liver and stored in the gallbladder. Bile acids emulsify fats, increasing their surface area for enzymatic breakdown. Liver dysfunction can impair bile production, leading to fat malabsorption and steatorrhea (fatty stools).
- Plasma Proteins: As previously mentioned, the liver synthesizes many essential plasma proteins, including albumin, clotting factors (fibrinogen, prothrombin), and others crucial for blood clotting and maintaining blood osmotic pressure.
- Blood Clotting Factors: Deficiencies in clotting factors due to liver disease significantly increase the risk of bleeding. EMTs need to be vigilant for signs of bleeding in patients with suspected liver dysfunction.
4. Storage and Reservoir Function:
The liver also serves as a storage depot for several essential nutrients and vitamins:
- Glycogen: The liver stores significant amounts of glycogen, providing a readily available source of glucose for the body.
- Vitamins and Minerals: The liver stores vitamins A, D, E, K, B12, and iron. Liver disease can lead to deficiencies in these vital nutrients.
- Blood Volume: The liver's large blood volume capacity helps regulate blood flow and pressure.
Clinical Implications of Liver Dysfunction in EMT Practice
Understanding the liver's diverse functions provides the foundation for recognizing and managing various conditions in pre-hospital care. Signs and symptoms of liver dysfunction can be subtle or dramatic, depending on the severity and underlying cause. EMTs should be alert for:
- Jaundice: Yellow discoloration of the skin and eyes, indicating impaired bilirubin metabolism.
- Ascites: Fluid accumulation in the abdominal cavity, often due to portal hypertension (increased pressure in the hepatic portal vein).
- Hepatic Encephalopathy: Neurological dysfunction due to the accumulation of ammonia in the blood. Symptoms can range from mild confusion to coma.
- Coagulopathy: Impaired blood clotting due to decreased synthesis of clotting factors. This manifests as easy bruising, prolonged bleeding, and spontaneous hemorrhage.
- Hypoglycemia: Low blood sugar due to impaired glucose metabolism.
- Edema: Fluid retention due to hypoalbuminemia (low albumin levels).
- Gastrointestinal Symptoms: Nausea, vomiting, diarrhea, abdominal pain, and changes in bowel habits.
Quizlet-Style Questions for EMTs
Let's test your knowledge with some quick-fire questions:
-
Which process involves the liver converting glucose into glycogen for storage? a) Glycogenolysis b) Gluconeogenesis c) Glycogenesis d) Lipolysis
-
What is the primary function of albumin, a protein synthesized by the liver? a) Blood clotting b) Maintaining blood osmotic pressure c) Detoxifying ammonia d) Transporting oxygen
-
Jaundice is a clinical sign of impaired metabolism of which substance? a) Glucose b) Ammonia c) Bilirubin d) Cholesterol
-
What is the most common cause of cirrhosis in the United States? a) Hepatitis A b) Hepatitis B c) Alcohol abuse d) Genetic predisposition
-
Which of the following is NOT a function of the liver? a) Detoxification of drugs b) Production of red blood cells c) Synthesis of clotting factors d) Metabolism of carbohydrates
Answer Key: 1. c, 2. b, 3. c, 4. c, 5. b
Conclusion: The Liver's Importance in EMT Practice
The liver’s crucial role in metabolism, detoxification, synthesis, and storage underscores its paramount importance in maintaining overall health. EMTs must be familiar with the liver's diverse functions and the potential clinical implications of its dysfunction. Recognizing the signs and symptoms of liver disease allows for prompt assessment, appropriate management, and potentially life-saving interventions. A thorough understanding of the liver's complex role empowers EMTs to provide optimal pre-hospital care for patients with various medical emergencies involving liver involvement. Continuous learning and refinement of knowledge on this vital organ are essential for competent and compassionate emergency medical service.
Latest Posts
Latest Posts
-
Compared To Terrestrial Planets Jovian Planets Are
Apr 02, 2025
-
Nurse Logic 2 0 Knowledge And Clinical Judgment Advanced Test
Apr 02, 2025
-
Which Of The Following Describe How To Communicate Pals
Apr 02, 2025
-
The Hair Below The Crest Is Known As The
Apr 02, 2025
-
Managerial Strategy Are The Odds In Atlantic Hotels Favor
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Functions Of The Liver Include Quizlet Emt . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
