Heart Failure With Atrial Fibrillation Hesi Case Study
Breaking News Today
Mar 20, 2025 · 6 min read
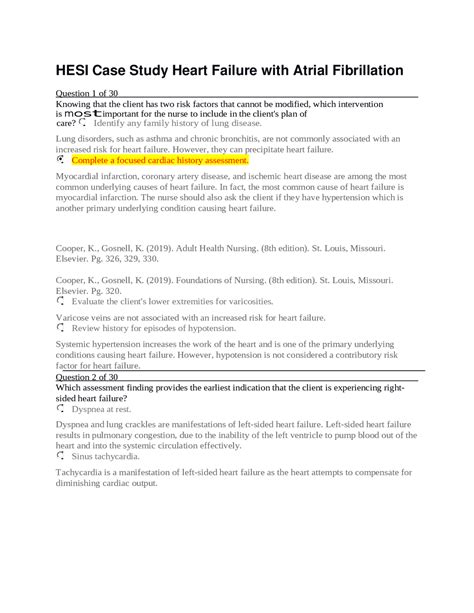
Table of Contents
Heart Failure with Atrial Fibrillation: A Comprehensive HESI Case Study Analysis
Heart failure (HF) coupled with atrial fibrillation (AFib) presents a complex clinical picture demanding meticulous assessment and management. This case study delves into a hypothetical patient scenario, exploring the pathophysiology, diagnostic workup, treatment strategies, and nursing implications associated with this challenging condition. We will use a HESI (Health Education Systems, Inc.) case study approach to analyze the multifaceted aspects of this intertwined pathology.
Understanding the Interplay of Heart Failure and Atrial Fibrillation
Before diving into the case study, let's establish a foundational understanding of both heart failure and atrial fibrillation, and how they interact to exacerbate patient morbidity.
Heart Failure: A Failing Pump
Heart failure is a clinical syndrome characterized by the heart's inability to effectively pump blood to meet the body's metabolic demands. This can stem from various underlying causes, including:
- Systolic dysfunction: The heart's inability to contract forcefully enough to eject sufficient blood volume.
- Diastolic dysfunction: The heart's inability to relax and fill properly during diastole, hindering blood filling.
- Valvular heart disease: Malfunctioning heart valves impede blood flow.
- Cardiomyopathies: Diseases affecting the heart muscle itself.
- Hypertension: Chronic high blood pressure strains the heart.
- Coronary artery disease: Reduced blood supply to the heart muscle.
Key symptoms of heart failure include dyspnea (shortness of breath), fatigue, edema (swelling), orthopnea (shortness of breath when lying flat), paroxysmal nocturnal dyspnea (sudden shortness of breath at night), and persistent cough.
Atrial Fibrillation: A Chaotic Rhythm
Atrial fibrillation is a common arrhythmia characterized by rapid, irregular, and disorganized electrical activity in the atria. This chaotic rhythm prevents the atria from effectively contracting, leading to several complications:
- Reduced cardiac output: Inefficient atrial contraction diminishes the amount of blood pumped to the ventricles.
- Thrombus formation: Stagnant blood in the atria increases the risk of blood clot formation.
- Stroke: Embolization of clots from the atria can lead to stroke.
- Heart failure exacerbation: Reduced cardiac output further burdens an already compromised heart.
Common symptoms of AFib include palpitations, dizziness, shortness of breath, and chest pain. Many individuals with AFib are asymptomatic.
The Synergistic Effect: HF and AFib Together
The combination of heart failure and atrial fibrillation creates a vicious cycle. AFib reduces cardiac output, further stressing a heart already struggling to meet the body's demands. This leads to increased symptoms of heart failure, reduced exercise tolerance, and a higher risk of serious complications like stroke. Managing both conditions concurrently is crucial for optimal patient outcomes.
The HESI Case Study: A Detailed Examination
Let's now consider a hypothetical HESI case study involving a patient with heart failure and atrial fibrillation:
Patient Profile: A 72-year-old male patient, Mr. Jones, presents to the emergency department with complaints of worsening shortness of breath, persistent cough, and fatigue over the past week. He has a history of hypertension, coronary artery disease, and type 2 diabetes mellitus. He reports a recent increase in his edema, particularly in his lower extremities.
Assessment Findings:
- Vitals: Blood pressure 160/90 mmHg, heart rate 120 bpm (irregular), respiratory rate 28 breaths/min, oxygen saturation 88% on room air.
- Cardiac Exam: Irregularly irregular rhythm, S3 gallop, bibasilar crackles.
- Pulmonary Exam: Diminished breath sounds at the bases.
- Edema: 2+ pitting edema in both lower extremities.
- Electrocardiogram (ECG): Atrial fibrillation with a rapid ventricular response.
- Chest X-ray: Cardiomegaly (enlarged heart), pulmonary edema.
- Blood tests: Elevated BNP (B-type natriuretic peptide), elevated creatinine.
Nursing Diagnoses:
Based on the assessment findings, the following nursing diagnoses are formulated:
- Ineffective Breathing Pattern related to pulmonary edema and increased cardiac workload.
- Decreased Cardiac Output related to impaired myocardial contractility and atrial fibrillation.
- Excess Fluid Volume related to heart failure.
- Risk for Thromboembolism related to atrial fibrillation.
- Activity Intolerance related to decreased cardiac output and fatigue.
Treatment Plan and Nursing Interventions
Mr. Jones's treatment plan will focus on addressing both his heart failure and atrial fibrillation:
Managing Heart Failure:
- Oxygen Therapy: Supplemental oxygen is crucial to improve oxygen saturation.
- Diuretics: To reduce fluid overload and pulmonary edema. Loop diuretics like furosemide are commonly used.
- ACE Inhibitors or ARBs: To reduce afterload and improve cardiac function. These medications help relax blood vessels.
- Beta-Blockers: To reduce heart rate and myocardial oxygen demand. Careful titration is required, especially in the presence of AFib.
- Digoxin: A cardiac glycoside that can improve contractility and heart rate control, but it's used less frequently now due to potential adverse effects.
Managing Atrial Fibrillation:
- Rate Control: If the ventricular rate is excessively high, medications like beta-blockers, calcium channel blockers, or digoxin are used to slow the heart rate.
- Rhythm Control: Antiarrhythmic drugs, such as amiodarone or flecainide, may be used to restore and maintain sinus rhythm. Cardioversion (electrical shock) may also be considered.
- Anticoagulation: Mr. Jones is at high risk for stroke due to AFib. Anticoagulants, such as warfarin, dabigatran, apixaban, or rivaroxaban, are essential to prevent thrombus formation and subsequent embolic events.
Nursing Interventions:
- Continuous monitoring of vital signs, including heart rate, rhythm, blood pressure, respiratory rate, and oxygen saturation.
- Assessment of lung sounds, edema, and daily weights.
- Administer medications as prescribed, carefully monitoring for adverse effects.
- Promote rest and reduce activity intolerance.
- Educate the patient and family about the disease process, medication regimen, and lifestyle modifications.
- Monitor for signs and symptoms of worsening heart failure or complications like pulmonary edema.
- Strict adherence to fluid restrictions as ordered.
- Encourage a low-sodium diet.
- Patient and family education regarding medication side effects, dietary restrictions, activity modifications, and signs and symptoms that warrant immediate medical attention.
- Emotional support and stress management techniques for patient and family coping.
Potential Complications and Monitoring
Close monitoring for potential complications is essential. These include:
- Pulmonary edema: Worsening shortness of breath, increased crackles in the lungs, and decreased oxygen saturation.
- Hypotension: Low blood pressure, dizziness, and lightheadedness.
- Electrolyte imbalances: Hypokalemia (low potassium), which can increase the risk of arrhythmias. Careful monitoring of serum electrolytes is crucial, especially when administering diuretics.
- Bleeding complications: With anticoagulant therapy, close monitoring for signs of bleeding is essential (bruising, bleeding gums, dark stools, etc.).
- Stroke: Sudden weakness or numbness on one side of the body, difficulty speaking, or vision changes.
Patient Education and Discharge Planning
Thorough patient and family education is critical for successful long-term management. This includes:
- Medication adherence: Understanding the purpose, dosage, timing, and potential side effects of each medication.
- Dietary modifications: A low-sodium diet, limiting fluid intake as prescribed, and choosing heart-healthy foods.
- Activity modifications: Gradual increase in activity as tolerated, avoiding strenuous exercise.
- Weight monitoring: Daily weights to detect fluid retention.
- Symptom monitoring: Recognizing and reporting worsening shortness of breath, edema, chest pain, or other concerning symptoms.
- Follow-up appointments: Importance of regular follow-up visits with the healthcare provider.
Conclusion: A Holistic Approach to a Complex Condition
Managing heart failure with atrial fibrillation requires a holistic, multidisciplinary approach. This case study highlights the crucial interplay between pathophysiology, diagnostic testing, treatment strategies, and nursing interventions. Effective collaboration among healthcare providers, coupled with diligent patient education and adherence to treatment plans, is essential for optimizing patient outcomes and improving quality of life for individuals facing this complex challenge. The continuous monitoring of vital signs, careful administration of medications, and diligent assessment for complications are paramount in ensuring the patient's safety and well-being. A focus on patient and family education empowers them to actively participate in their care, significantly enhancing long-term management and reducing the risk of future exacerbations. Understanding the underlying pathophysiology and the potential synergistic effects of heart failure and atrial fibrillation is crucial for successful clinical management.
Latest Posts
Latest Posts
-
Nihss Certification Nihss Answer Key Group B
Mar 20, 2025
-
Which Best Describes A Drama Written In An Experimental Style
Mar 20, 2025
-
Children And Adults Can Both Benefit From Having A Dietician
Mar 20, 2025
-
Why Is Cumulative Risk A Serious Concern
Mar 20, 2025
-
Foundations In Health And Safety E Learning Post Test Answers
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Heart Failure With Atrial Fibrillation Hesi Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
