Match Each Erythrocyte Disorder To Its Cause Or Definition
Breaking News Today
Mar 15, 2025 · 7 min read
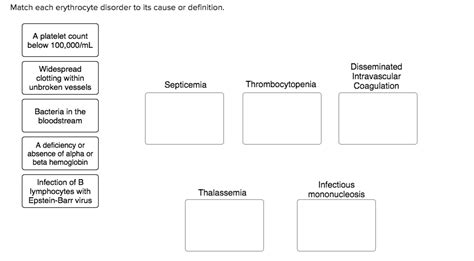
Table of Contents
Matching Erythrocyte Disorders to Their Causes and Definitions
Erythrocytes, also known as red blood cells (RBCs), are the most abundant cells in the blood, playing a vital role in oxygen transport throughout the body. Disruptions in their production, function, or destruction can lead to a wide range of disorders, each with its unique cause and clinical presentation. This comprehensive guide will delve into various erythrocyte disorders, meticulously matching each condition to its underlying cause or definition. We will explore the pathophysiology, clinical manifestations, and diagnostic approaches associated with these conditions.
I. Disorders of Erythrocyte Production (Erythropoiesis)
Erythropoiesis, the process of red blood cell production, is a tightly regulated process that can be disrupted by various factors, leading to decreased red blood cell count (anemia) or abnormalities in red blood cell morphology.
A. Aplastic Anemia
Definition: Aplastic anemia is a rare and severe condition characterized by the failure of the bone marrow to produce sufficient numbers of all three major blood cell types: red blood cells, white blood cells, and platelets.
Cause: The exact cause of aplastic anemia is often unknown (idiopathic), but it can be triggered by:
- Genetic factors: Certain inherited conditions can predispose individuals to aplastic anemia.
- Autoimmune diseases: The body's immune system mistakenly attacks and destroys the hematopoietic stem cells in the bone marrow.
- Exposure to toxins: Exposure to chemicals such as benzene, certain medications, and radiation can damage the bone marrow.
- Viral infections: Some viral infections, such as Epstein-Barr virus (EBV) and parvovirus B19, have been implicated in the development of aplastic anemia.
Clinical Manifestations: Aplastic anemia manifests with fatigue, weakness, pallor, shortness of breath, frequent infections, easy bruising, and prolonged bleeding.
B. Anemia of Chronic Disease (ACD)
Definition: Anemia of chronic disease is a common type of anemia associated with chronic inflammatory conditions, infections, and malignancies.
Cause: ACD arises from a complex interplay of factors, including:
- Decreased erythropoietin production: Inflammation suppresses the production of erythropoietin, a hormone that stimulates red blood cell production.
- Shorter red blood cell lifespan: Inflammatory cytokines shorten the lifespan of red blood cells, leading to increased destruction.
- Impaired iron utilization: Iron is trapped in macrophages, making it unavailable for red blood cell production.
Clinical Manifestations: Symptoms of ACD are often subtle and may include fatigue, weakness, and pallor. Severity depends on the underlying chronic condition.
C. Iron Deficiency Anemia
Definition: Iron deficiency anemia is the most common type of anemia worldwide, characterized by a deficiency of iron, a crucial component of hemoglobin.
Cause: Iron deficiency anemia typically results from:
- Inadequate iron intake: Insufficient dietary iron intake, particularly common in vegetarians or individuals with poor nutrition.
- Increased iron demand: Periods of rapid growth, pregnancy, and lactation increase iron requirements.
- Blood loss: Chronic blood loss, from sources such as heavy menstrual bleeding, gastrointestinal bleeding, or internal bleeding, can deplete iron stores.
- Malabsorption: Conditions affecting iron absorption in the intestines, such as celiac disease or Crohn's disease.
Clinical Manifestations: Iron deficiency anemia can present with fatigue, weakness, pallor, shortness of breath, palpitations, and brittle nails. In severe cases, spoon-shaped nails (koilonychia) and a smooth, sore tongue (glossitis) may be observed.
D. Megaloblastic Anemia
Definition: Megaloblastic anemia is a type of anemia characterized by the presence of large, immature red blood cells (megaloblasts) in the bone marrow and blood.
Cause: Megaloblastic anemia is primarily caused by deficiencies in vitamin B12 (cobalamin) or folate (folic acid), both essential for DNA synthesis and red blood cell maturation.
- Vitamin B12 deficiency: Can result from pernicious anemia (autoimmune destruction of parietal cells in the stomach), dietary deficiency (rare in developed countries), or malabsorption syndromes.
- Folate deficiency: Can result from dietary deficiency, malabsorption, or increased folate requirements (pregnancy, lactation).
Clinical Manifestations: Symptoms include fatigue, weakness, pallor, shortness of breath, neurological symptoms (numbness, tingling, difficulty walking – particularly in B12 deficiency), and glossitis.
E. Thalassemia
Definition: Thalassemia is a group of inherited blood disorders characterized by reduced or absent synthesis of globin chains, the protein components of hemoglobin.
Cause: Thalassemia results from genetic mutations affecting the genes responsible for producing globin chains. The severity varies depending on the type and extent of the mutation.
- Alpha-thalassemia: Reduced or absent production of alpha-globin chains.
- Beta-thalassemia: Reduced or absent production of beta-globin chains.
Clinical Manifestations: Symptoms range from mild anemia to severe anemia requiring regular blood transfusions. Severe forms can lead to bone deformities, growth retardation, and organ damage.
II. Disorders of Erythrocyte Function
These disorders affect the ability of red blood cells to carry and deliver oxygen effectively.
A. Sickle Cell Anemia
Definition: Sickle cell anemia is an inherited blood disorder characterized by abnormal hemoglobin S (HbS), which causes red blood cells to become rigid, sickle-shaped, and prone to clumping.
Cause: Sickle cell anemia is caused by a genetic mutation in the beta-globin gene, leading to the production of HbS. Individuals inherit two copies of the mutated gene (homozygous) to have sickle cell anemia.
Clinical Manifestations: The hallmark symptom is recurrent painful episodes (vaso-occlusive crises) caused by the blockage of blood vessels by sickled red blood cells. Other manifestations include anemia, infections, organ damage, and acute chest syndrome.
B. Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency
Definition: G6PD deficiency is an X-linked inherited enzyme deficiency that affects red blood cell stability.
Cause: A genetic defect reduces or eliminates the activity of the G6PD enzyme, which plays a crucial role in protecting red blood cells from oxidative damage.
Clinical Manifestations: Individuals with G6PD deficiency are usually asymptomatic unless exposed to oxidative stressors such as certain drugs, infections, or fava beans. This can trigger hemolytic anemia, characterized by the premature destruction of red blood cells, leading to jaundice, fatigue, and dark urine.
III. Disorders of Erythrocyte Destruction (Hemolysis)
These disorders result from the increased destruction of red blood cells.
A. Autoimmune Hemolytic Anemia
Definition: Autoimmune hemolytic anemia is a condition in which the body's immune system mistakenly attacks and destroys its own red blood cells.
Cause: The immune system produces antibodies that bind to red blood cell surface antigens, leading to their destruction by the spleen and liver. This can be triggered by various factors, including infections, autoimmune diseases, or certain medications.
Clinical Manifestations: Symptoms include anemia, jaundice, fatigue, and splenomegaly (enlarged spleen).
B. Hereditary Spherocytosis
Definition: Hereditary spherocytosis is an inherited disorder characterized by the production of abnormally small and spherical red blood cells (spherocytes).
Cause: Genetic defects affecting proteins involved in maintaining the structural integrity of the red blood cell membrane lead to the formation of spherocytes, which are more fragile and prone to destruction.
Clinical Manifestations: Symptoms include anemia, jaundice, splenomegaly, and gallstones.
C. Paroxysmal Nocturnal Hemoglobinuria (PNH)
Definition: PNH is a rare, acquired disorder characterized by the destruction of red blood cells, white blood cells, and platelets due to a defect in the complement regulatory protein.
Cause: Somatic mutations affecting the PIGA gene lead to a deficiency in glycosylphosphatidylinositol (GPI)-anchored proteins on the surface of blood cells, making them susceptible to complement-mediated destruction.
Clinical Manifestations: PNH is characterized by recurrent episodes of hemoglobinuria (hemoglobin in the urine), hemolytic anemia, venous thrombosis, and cytopenias (low blood cell counts).
D. Hemolytic Disease of the Newborn (HDN)
Definition: HDN, also known as erythroblastosis fetalis, is a condition in which the mother's antibodies attack the red blood cells of her fetus.
Cause: HDN occurs when the mother is Rh-negative and the fetus is Rh-positive. During pregnancy or delivery, fetal Rh-positive red blood cells can enter the mother's circulation, triggering the production of anti-Rh antibodies. In subsequent pregnancies with an Rh-positive fetus, these maternal antibodies can cross the placenta and destroy fetal red blood cells.
Clinical Manifestations: Severity varies but can range from mild jaundice to severe anemia, heart failure, and even death.
Conclusion
This comprehensive overview highlights the diverse spectrum of erythrocyte disorders, emphasizing their underlying causes and defining characteristics. Understanding the pathophysiology of these disorders is critical for accurate diagnosis, appropriate management, and improved patient outcomes. While this article provides a broad overview, consulting with a healthcare professional for diagnosis and treatment is essential for any suspected erythrocyte disorder. Further research into specific conditions will uncover even more nuanced details about their etiology and management, highlighting the ongoing importance of hematological research. The intricate interplay of genetics, immune function, and environmental factors in shaping these disorders underscores the complexity of human physiology and the importance of personalized medicine approaches. Continued advancements in diagnostic techniques and therapeutic strategies are crucial in improving the lives of individuals affected by these conditions. Early diagnosis and proactive management are key to mitigating the long-term complications associated with these diverse disorders, emphasizing the importance of regular health screenings and prompt medical attention when symptoms arise.
Latest Posts
Latest Posts
-
The Discharge Category Which Indicates Satisfactory Service
Mar 15, 2025
-
How Did Elevated Trains And Subways Improve Urban Transportation
Mar 15, 2025
-
Siphoning Of Wetlands In Iraq Has Led To
Mar 15, 2025
-
Patients With Perfusing Rhythms Should Receive Ventilations Once Every
Mar 15, 2025
-
In A State Supervised County Administered State
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about Match Each Erythrocyte Disorder To Its Cause Or Definition . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
