Medical Ethics And Detainee Operations Basic Course Pretest
Breaking News Today
Mar 26, 2025 · 7 min read
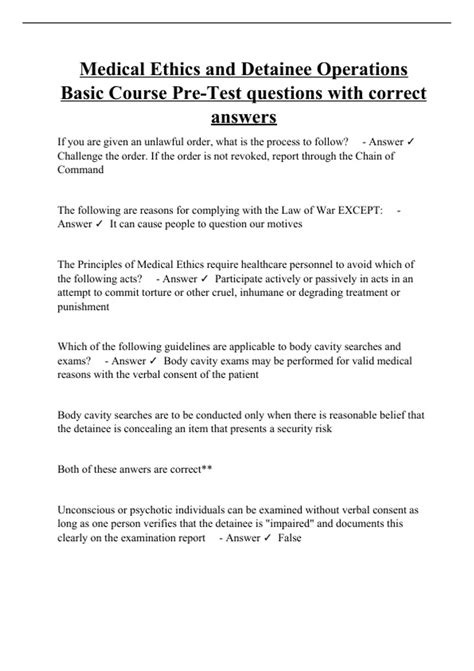
Table of Contents
Medical Ethics and Detainee Operations Basic Course Pretest: A Comprehensive Guide
The Medical Ethics and Detainee Operations Basic Course is a crucial training program for medical professionals involved in detainee care. This course covers a wide range of ethical considerations and practical challenges faced in this sensitive area. Before embarking on this important training, a pretest is often administered to assess existing knowledge and identify areas requiring further focus. This article serves as a comprehensive guide covering potential pretest questions, key ethical concepts, and the practical implications of providing medical care in detainee settings.
Understanding the Context: Medical Ethics in Detainee Operations
The ethical challenges in detainee care are multifaceted and complex. Medical professionals must navigate a landscape shaped by legal frameworks, humanitarian principles, and the inherent vulnerabilities of the detained population. The core tenets of medical ethics – beneficence, non-maleficence, autonomy, and justice – are constantly tested in this environment. These principles are not mutually exclusive; often, they come into conflict, demanding careful consideration and a nuanced approach.
Beneficence: Maximizing Benefit and Minimizing Harm
Beneficence mandates that healthcare providers act in the best interests of their patients. In detainee operations, this means providing high-quality medical care, promptly addressing health concerns, and advocating for the well-being of individuals in custody. This principle faces several challenges, such as limited resources, challenging environments, and potential conflicts of interest arising from the detainee's status. What constitutes "best interests" in a context of detention? This is a critical ethical question that requires careful examination.
Non-Maleficence: Avoiding Harm
Non-maleficence, the principle of "do no harm," is paramount in medicine. In detainee settings, this extends beyond physical harm to include psychological harm, exploitation, and the potential for mistreatment. Medical professionals have a responsibility to ensure that their actions do not contribute to the suffering or degradation of detainees. How can medical personnel ensure they are not complicit in inhumane treatment? This question underlines the importance of understanding legal and ethical boundaries.
Autonomy: Respecting Patient Rights
Respecting the autonomy of detainees is fundamental to ethical medical practice. This involves obtaining informed consent before any medical procedure or treatment, respecting their choices about their care, and ensuring their right to confidentiality. However, the constraints of detention – including limitations on freedom of movement and communication – can significantly impact the ability to uphold patient autonomy. How can informed consent be effectively obtained in a setting where individual liberty is restricted? This issue demands creative solutions that balance respect for autonomy with the realities of the operational context.
Justice: Equitable and Fair Treatment
The principle of justice requires fair and equitable treatment of all individuals. In detainee operations, this means ensuring that detainees receive the same standard of medical care as any other patient, regardless of their status, background, or alleged offenses. How can healthcare providers ensure equitable distribution of resources and prevent discrimination in detainee settings? Addressing this challenge requires robust systems for resource allocation and a commitment to impartiality.
Potential Pretest Questions and Answers:
This section offers examples of potential questions that might appear on a Medical Ethics and Detainee Operations Basic Course pretest. Remember, these are illustrative examples and the actual questions on any given pretest will vary.
1. A detainee refuses medical treatment for a potentially life-threatening condition. What is the most ethically sound approach?
- Answer: While respecting the detainee's autonomy, explore the reasons for refusal, provide information about the condition and treatment options, and document the conversation thoroughly. Depending on the severity of the condition and the risk of harm, legal counsel may be necessary to consider alternatives. Forced treatment is generally unethical unless there's an imminent threat to life and no less restrictive alternative exists.
2. You suspect a detainee is being subjected to torture. What are your ethical and legal obligations?
- Answer: You have a strong ethical and potentially legal obligation to report suspected torture. This should be done through appropriate channels, ensuring your safety and potentially the safety of the detainee. Document all observations and concerns meticulously. Failure to report such suspicions constitutes a serious breach of medical ethics.
3. A detainee requests access to a specific medication not readily available in the facility. What considerations should guide your response?
- Answer: Assess the medical necessity of the medication. Explore whether a suitable alternative is available. If the medication is medically necessary and not available, advocate for its procurement, balancing the detainee's needs with the operational constraints. This might involve contacting relevant authorities and escalating the request through appropriate channels.
4. You are asked to participate in an interrogation of a detainee. What is your ethical response?
- Answer: Refuse. Medical professionals should not participate in interrogations or any activity that compromises their ethical obligations or could be perceived as contributing to torture or coercion. Your role is to provide impartial medical care, not to facilitate interrogation or other non-medical functions.
5. A detainee discloses sensitive personal information during a medical consultation. What are your responsibilities regarding confidentiality?
- Answer: Maintain confidentiality to the greatest extent possible. However, exceptions exist in situations where there is a serious risk of harm to the detainee or others (e.g., a credible threat of violence). In such cases, appropriate legal and ethical guidelines must be followed when disclosing information.
6. Limited resources are available for medical care in the detainee facility. How should you prioritize care?
- Answer: Utilize a triage system based on medical urgency, prioritizing individuals with life-threatening conditions. Transparency in resource allocation is crucial. This requires a clear and well-defined system to ensure equitable distribution of limited resources.
7. You observe a colleague acting unethically in their treatment of a detainee. What actions should you take?
- Answer: Document the incident thoroughly and, depending on the severity, report the unethical behavior through appropriate channels within the facility. If the issue involves potential harm, immediate action may be required to prevent further harm. Involving a supervisor or other appropriate authorities is often essential.
8. What is the difference between medical necessity and medical appropriateness in the context of detainee care?
- Answer: Medical necessity refers to the essential treatment required to address a detainee’s immediate health needs, while medical appropriateness refers to the suitability of the treatment provided within the context of the available resources and ethical standards. Sometimes, a treatment might be medically appropriate but not medically necessary in a particular situation.
9. How does the Geneva Conventions impact ethical considerations in detainee care?
- Answer: The Geneva Conventions provide a legal framework that outlines the humane treatment of detainees, including access to medical care. They prohibit torture, cruel, inhuman, or degrading treatment, and underscore the medical professional's ethical duty to uphold these standards. Compliance with the Geneva Conventions guides ethical decision-making in detainee care.
10. What are the key differences between a POW (Prisoner of War) and a civilian detainee in terms of medical ethics?
- Answer: While both groups are entitled to humane treatment and access to medical care, POWs have additional protections under the Geneva Conventions, including specific provisions regarding their status, treatment, and repatriation. Medical ethics applied to POWs must align with the specific requirements and protections outlined in the Geneva Conventions.
Conclusion: Preparing for Ethical Challenges
The Medical Ethics and Detainee Operations Basic Course Pretest is a vital tool for assessing and enhancing the ethical preparedness of medical professionals working in detainee settings. By understanding the core principles of medical ethics, anticipating potential conflicts, and preparing for challenging situations, medical personnel can ensure they provide high-quality, ethical, and humane care within the complex framework of detainee operations. The ethical considerations outlined in this guide are fundamental to maintaining professional integrity and upholding the highest standards of medical practice in challenging environments. Thorough preparation and ongoing reflection are critical for navigating the ethical complexities inherent in this specialized field.
Latest Posts
Latest Posts
-
Apply The Single Accounting Underline Format To The Selected Cells
Mar 29, 2025
-
Rn Learning System Medical Surgical Musculoskeletal Practice Quiz
Mar 29, 2025
-
Swimming Burns More Calories Per Hour Than Aerobics And Cycling
Mar 29, 2025
-
Nos Alojamos En Un Hotel Malo De La Capital
Mar 29, 2025
-
From A Security Perspective The Best Rooms Are
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Medical Ethics And Detainee Operations Basic Course Pretest . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
