Myasthenia Gravis Is An Autoimmune Disease In Which Quizlet
Breaking News Today
Mar 18, 2025 · 7 min read
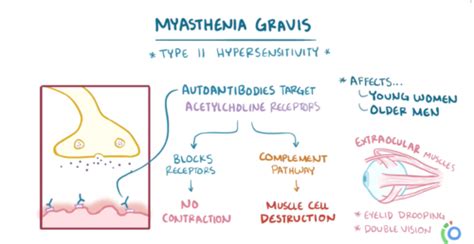
Table of Contents
Myasthenia Gravis: An Autoimmune Disease – A Comprehensive Overview
Myasthenia gravis (MG) is a chronic autoimmune neuromuscular disease characterized by varying degrees of weakness and fatigability of the voluntary muscles. It's a complex condition, and understanding its intricacies is crucial for effective management and improved quality of life for those affected. This in-depth exploration delves into the disease's pathogenesis, symptoms, diagnosis, treatment, and ongoing research, aiming to provide a comprehensive understanding of myasthenia gravis.
Understanding the Autoimmune Nature of Myasthenia Gravis
At the heart of myasthenia gravis lies an autoimmune response. The body's immune system, designed to protect against foreign invaders, mistakenly attacks its own tissues. In MG, the target is the acetylcholine receptors (AChRs) located at the neuromuscular junction – the point where nerve impulses transmit to muscles.
The Role of Antibodies and the Neuromuscular Junction
The immune system produces autoantibodies, specifically antibodies targeting the AChRs. These antibodies bind to the receptors, blocking or destroying them. This disruption significantly impairs the transmission of nerve impulses to the muscles, leading to the characteristic muscle weakness and fatigue. The severity of the disease depends on the number of AChRs affected and the extent of the disruption at the neuromuscular junction.
Other Autoantibodies and Their Impact
While AChR antibodies are the most common, other autoantibodies can also play a role in MG. These include antibodies against muscle-specific kinase (MuSK) and lipoprotein-related protein 4 (LRP4). These antibodies target different components of the neuromuscular junction and can contribute to the disease's development and progression. The presence and type of autoantibodies can influence the diagnosis, prognosis, and treatment strategy for individual patients.
Recognizing the Symptoms of Myasthenia Gravis
The symptoms of myasthenia gravis are highly variable, ranging from mild to severe, and can fluctuate throughout the day. Fatigue often worsens with activity and improves with rest. The most common symptoms include:
Muscular Weakness and Fatigue
Muscle weakness is a hallmark of MG. It typically affects the muscles that control eye movement, facial expression, chewing, swallowing, and speech. This weakness is often described as fluctuating, meaning it can vary in severity throughout the day. Fatigue is another prominent feature, disproportionately affecting muscles after periods of activity.
Ocular Myasthenia Gravis
Ocular myasthenia gravis involves weakness of the eye muscles. This can manifest as:
- Ptosis: Drooping of one or both eyelids.
- Diplopia: Double vision.
These symptoms are often the first signs of the disease, and some individuals experience only ocular involvement.
Generalized Myasthenia Gravis
Generalized myasthenia gravis affects muscles beyond the eyes. This can include:
- Facial weakness: Difficulty smiling, frowning, or chewing.
- Bulbar weakness: Weakness of the muscles involved in swallowing and speech, leading to dysphagia (difficulty swallowing) and dysarthria (difficulty speaking).
- Limb weakness: Weakness in the arms and legs.
- Respiratory muscle weakness: In severe cases, weakness of the respiratory muscles can lead to respiratory failure, a life-threatening complication.
Fluctuating Nature of Symptoms
It's crucial to remember that the symptoms of myasthenia gravis are often fluctuating. They may worsen with exertion, heat, stress, or illness, and improve with rest. This fluctuation can make diagnosis challenging, and it's essential for individuals to maintain close communication with their healthcare providers.
Diagnosing Myasthenia Gravis: A Multifaceted Approach
Diagnosing myasthenia gravis requires a comprehensive evaluation that combines clinical assessment, neurological examination, and various diagnostic tests.
Clinical Evaluation and Neurological Examination
The diagnosis begins with a thorough clinical evaluation and neurological examination. The doctor will assess the patient's medical history, symptoms, and the pattern of muscle weakness. The neurological examination focuses on evaluating muscle strength, reflexes, and sensory function.
The Tensilon Test (Edrophonium Test)
The Tensilon test (edrophonium test) is a crucial diagnostic tool. Edrophonium is a short-acting acetylcholinesterase inhibitor. It temporarily increases the amount of acetylcholine at the neuromuscular junction, improving muscle strength. A positive Tensilon test, demonstrating significant improvement in muscle strength after edrophonium administration, strongly suggests MG.
Electromyography (EMG) and Repetitive Nerve Stimulation (RNS)
Electromyography (EMG) assesses the electrical activity of muscles. Repetitive nerve stimulation (RNS) involves stimulating a nerve repeatedly and measuring the muscle response. In MG, the muscle response gradually decreases with repeated stimulation, a phenomenon known as decrement.
Blood Tests for Autoantibodies
Blood tests are used to detect the presence of autoantibodies targeting AChR, MuSK, and LRP4. The presence of these antibodies helps confirm the diagnosis. However, it’s important to note that some individuals with MG may have negative antibody tests.
Imaging Studies
While not routinely used for diagnosis, imaging studies like computed tomography (CT) or magnetic resonance imaging (MRI) might be employed to rule out other conditions or identify potential complications.
Managing Myasthenia Gravis: Treatment Strategies
The management of myasthenia gravis aims to alleviate symptoms, improve quality of life, and prevent life-threatening complications. Treatment strategies often involve a combination of therapies tailored to the individual's needs.
Cholinesterase Inhibitors
Cholinesterase inhibitors, such as pyridostigmine and neostigmine, are the cornerstone of MG treatment. These medications inhibit the breakdown of acetylcholine, increasing its availability at the neuromuscular junction and improving muscle strength.
Immunosuppressive Therapy
Immunosuppressive therapies aim to suppress the immune system's attack on the AChRs. These medications can include corticosteroids (prednisone), azathioprine, mycophenolate mofetil, cyclosporine, and rituximab. The choice of immunosuppressant depends on the individual's condition and response to treatment.
Thymectomy
Thymectomy, the surgical removal of the thymus gland, is a beneficial treatment option for many MG patients, particularly those with generalized MG and thymic hyperplasia (enlargement of the thymus). The thymus gland plays a significant role in the development of the autoimmune response in MG.
Plasmapheresis and Intravenous Immunoglobulin (IVIg)
Plasmapheresis removes antibodies from the blood, providing temporary symptom relief. Intravenous immunoglobulin (IVIg), a concentrated solution of antibodies from healthy donors, also offers short-term symptomatic improvement. These treatments are often used during periods of severe exacerbations.
Other Treatments and Supportive Care
Other treatments may include medications to manage specific symptoms such as respiratory support for respiratory weakness, eye drops for dry eyes associated with ptosis, and physical therapy to maintain muscle strength and function. Supportive care plays a crucial role in improving the quality of life for individuals with MG. This includes education about the condition, lifestyle adjustments, and psychosocial support.
Living with Myasthenia Gravis: Coping and Long-Term Management
Living with myasthenia gravis requires a multifaceted approach that combines medical management, lifestyle adjustments, and emotional well-being.
Lifestyle Adaptations and Self-Management
Individuals with MG need to make certain lifestyle adjustments to manage their symptoms and prevent exacerbations. These might include:
- Energy conservation techniques: Planning activities to avoid overexertion.
- Avoiding triggers: Identifying and minimizing exposure to factors that worsen symptoms (stress, heat, illness).
- Regular exercise: Maintaining physical fitness within the limits of their condition.
- Healthy diet: Maintaining a balanced diet to support overall health.
Emotional and Psychological Well-being
Living with a chronic autoimmune condition can be challenging, leading to stress, anxiety, and depression. Access to psychological support services, such as counseling or support groups, can significantly improve the emotional well-being of individuals with MG.
Importance of Regular Monitoring
Regular monitoring by a healthcare team is essential for managing myasthenia gravis. This involves regular appointments, ongoing assessment of symptoms, adjustments to medication as needed, and prompt management of any complications.
Ongoing Research and Future Directions in Myasthenia Gravis
Research into myasthenia gravis is ongoing, with several promising avenues of investigation. These include:
Novel Immunotherapies
Researchers are actively exploring novel immunotherapies aimed at modulating the immune response more precisely and effectively, reducing side effects, and improving long-term outcomes.
Understanding Disease Pathogenesis
Further research into the underlying pathogenesis of myasthenia gravis is crucial for developing more effective and targeted therapies. This includes investigations into the specific roles of different autoantibodies and the genetic factors contributing to disease susceptibility.
Biomarkers and Diagnostic Tools
The development of more sensitive and specific biomarkers and diagnostic tools will improve the early detection and diagnosis of MG, leading to earlier intervention and better outcomes.
Personalized Medicine Approaches
The future of MG management likely lies in personalized medicine approaches, tailoring treatment strategies to the individual's genetic profile, autoantibody profile, and disease severity.
Myasthenia gravis is a complex autoimmune disease requiring a comprehensive and individualized approach to management. Understanding the disease's pathogenesis, symptoms, diagnosis, and treatment options is crucial for improving the quality of life for those affected. Continued research offers hope for the development of novel therapies and improved long-term outcomes for individuals living with myasthenia gravis. This detailed overview should provide a solid foundation for understanding this challenging but manageable condition.
Latest Posts
Latest Posts
-
The Following Should Be Considered When Assessing Risk
Mar 18, 2025
-
A Changing Space Zone Is One That Is
Mar 18, 2025
-
When The Simcell Membrane In The Cell O Scope
Mar 18, 2025
-
The Shaft Of A Long Bone Is The
Mar 18, 2025
-
The Image Seen In A Plane Mirror Is Located
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Myasthenia Gravis Is An Autoimmune Disease In Which Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
