Pulmonary Edema And Impaired Ventilation Occur During:
Breaking News Today
Apr 01, 2025 · 6 min read
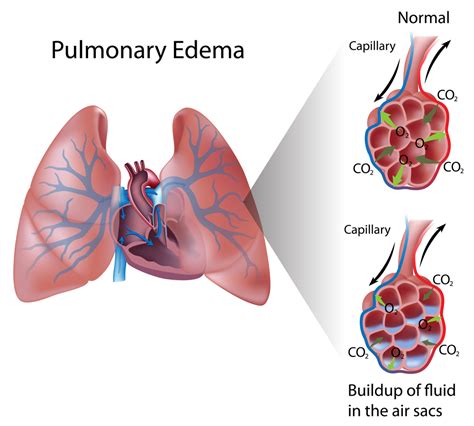
Table of Contents
Pulmonary Edema and Impaired Ventilation: A Comprehensive Overview
Pulmonary edema, characterized by fluid accumulation in the air sacs of the lungs, and impaired ventilation, a reduction in the efficiency of gas exchange, are serious medical conditions often intertwined. Understanding when these conditions occur together is crucial for effective diagnosis and treatment. This article explores the various scenarios where pulmonary edema and impaired ventilation present concurrently, delving into the underlying mechanisms and associated clinical manifestations.
Understanding Pulmonary Edema
Pulmonary edema arises when the delicate balance between fluid filtration from the pulmonary capillaries into the interstitial space and fluid reabsorption into the capillaries is disrupted. This imbalance leads to an excess of fluid in the alveoli (air sacs) and interstitium (tissue surrounding the alveoli), impairing gas exchange. There are two main types:
-
Cardiogenic Pulmonary Edema: This is the most common type and stems from heart failure. A weakened heart struggles to pump blood effectively, causing increased pressure in the pulmonary veins and capillaries. This elevated pressure forces fluid into the lungs. Symptoms often include shortness of breath, especially when lying down (orthopnea), and coughing up frothy, pink sputum.
-
Non-Cardiogenic Pulmonary Edema: This type arises from causes other than heart failure. Examples include:
-
Acute Respiratory Distress Syndrome (ARDS): ARDS is a severe lung injury characterized by widespread inflammation and fluid leakage into the alveoli. Multiple factors can trigger ARDS, including sepsis, pneumonia, trauma, and aspiration.
-
High-Altitude Pulmonary Edema (HAPE): At high altitudes, the reduced partial pressure of oxygen triggers the body to increase pulmonary blood flow, potentially leading to fluid leakage into the lungs.
-
Inhalation Injury: Inhaling toxic fumes or smoke can damage the alveolar-capillary membrane, causing fluid to leak into the alveoli.
-
Drug overdose: Certain medications, particularly opioids, can depress respiration and contribute to fluid accumulation in the lungs.
-
Understanding Impaired Ventilation
Impaired ventilation refers to a decrease in the efficiency of gas exchange between the lungs and the bloodstream. This can be caused by a variety of factors affecting either the mechanics of breathing (ventilation) or the diffusion of gases across the alveolar-capillary membrane. Several processes can lead to impaired ventilation:
-
Obstructive Lung Diseases: Conditions like asthma, chronic bronchitis, and emphysema obstruct airflow, limiting the amount of oxygen reaching the alveoli and hindering the removal of carbon dioxide.
-
Restrictive Lung Diseases: Diseases like pulmonary fibrosis and sarcoidosis restrict lung expansion, reducing the volume of air inhaled and exhaled.
-
Neuromuscular Disorders: Conditions affecting the nerves and muscles responsible for breathing, such as amyotrophic lateral sclerosis (ALS) and muscular dystrophy, can weaken respiratory muscles, leading to inadequate ventilation.
-
Central Nervous System Disorders: Brain injuries, strokes, or drug overdoses can affect the respiratory centers in the brainstem, leading to irregular or insufficient breathing.
Pulmonary Edema and Impaired Ventilation: Concurrent Occurrence
The simultaneous occurrence of pulmonary edema and impaired ventilation is often a critical medical situation requiring immediate intervention. The conditions frequently exacerbate each other, creating a vicious cycle. Here's how they interact:
-
Cardiogenic Pulmonary Edema and Impaired Ventilation: In heart failure, the increased pulmonary capillary pressure leading to edema also reduces the alveolar space available for gas exchange. The fluid accumulation directly interferes with the diffusion of oxygen into the blood and carbon dioxide out of the blood. Furthermore, the resulting shortness of breath and fatigue can further impair ventilation by limiting respiratory effort.
-
ARDS and Impaired Ventilation: ARDS is characterized by both severe pulmonary edema and significant impairment of gas exchange due to the widespread damage to the alveolar-capillary membrane. The fluid filling the alveoli physically blocks the passage of oxygen and carbon dioxide, resulting in severe hypoxemia (low blood oxygen levels) and hypercapnia (elevated blood carbon dioxide levels). The inflammatory process also contributes to impaired ventilation by causing bronchoconstriction and reducing lung compliance (ability to expand).
-
High-Altitude Pulmonary Edema (HAPE) and Impaired Ventilation: At high altitudes, the reduced oxygen pressure can trigger pulmonary edema. Simultaneously, the reduced oxygen levels themselves impair ventilation by limiting the driving force for oxygen diffusion across the alveolar-capillary membrane. The resulting hypoxemia can further exacerbate the pulmonary edema.
-
Inhalation Injury and Impaired Ventilation: Inhalation of toxic substances causes direct damage to the lung tissue, resulting in both pulmonary edema and impaired ventilation. The inflammation and edema obstruct airflow, while the damaged alveolar-capillary membrane hinders gas exchange.
-
Pneumonia and Impaired Ventilation: Pneumonia, an infection of the lungs, causes inflammation and fluid accumulation in the alveoli. This leads to both pulmonary edema and impaired ventilation. The inflammatory response and the presence of infectious material in the alveoli directly impair gas exchange. The body's response to the infection can also lead to bronchospasm, further restricting airflow.
Clinical Manifestations of Concurrent Pulmonary Edema and Impaired Ventilation
The clinical presentation of concurrent pulmonary edema and impaired ventilation is often severe and requires prompt medical attention. Common signs and symptoms include:
-
Severe shortness of breath (dyspnea): This is a hallmark symptom, often accompanied by increased respiratory rate and effort.
-
Cough: Cough may be dry or productive, producing frothy, pink-tinged sputum in cases of cardiogenic pulmonary edema.
-
Wheezing: Wheezing may indicate bronchospasm, often seen in asthma or other obstructive lung diseases.
-
Crackles (rales): These are abnormal breath sounds heard on auscultation (listening with a stethoscope) and indicate fluid in the lungs.
-
Cyanosis: A bluish discoloration of the skin and mucous membranes due to low blood oxygen levels.
-
Hypotension (low blood pressure): This can occur in severe cases, especially in cardiogenic pulmonary edema.
-
Tachycardia (rapid heart rate): The body compensates for low blood oxygen levels by increasing the heart rate.
-
Confusion or altered mental status: Severe hypoxemia can affect brain function.
-
Decreased oxygen saturation (SpO2): Measured using pulse oximetry, SpO2 reflects the percentage of hemoglobin saturated with oxygen. Low SpO2 indicates hypoxemia.
-
Increased carbon dioxide levels (PaCO2): Measured through arterial blood gas analysis, elevated PaCO2 indicates impaired ventilation and respiratory acidosis.
Diagnosis and Treatment
Diagnosing concurrent pulmonary edema and impaired ventilation often involves a combination of clinical evaluation, imaging studies, and blood tests. Key diagnostic tools include:
-
Chest X-ray: Shows fluid accumulation in the lungs and can help identify the extent of the edema.
-
Computed Tomography (CT) scan: Provides a more detailed image of the lungs, helpful in assessing the severity and distribution of the edema.
-
Arterial blood gas analysis: Measures blood oxygen and carbon dioxide levels, providing essential information about gas exchange.
-
Echocardiogram: Assesses heart function and helps differentiate cardiogenic from non-cardiogenic pulmonary edema.
Treatment strategies focus on addressing the underlying cause and supporting respiratory and circulatory function. Common interventions include:
-
Oxygen therapy: To improve blood oxygen levels.
-
Mechanical ventilation: For severe cases requiring respiratory support.
-
Diuretics: To remove excess fluid from the lungs in cardiogenic pulmonary edema.
-
Positive end-expiratory pressure (PEEP): A ventilator setting that helps keep the alveoli open and improve gas exchange.
-
Inotropic medications: To improve heart function in cardiogenic pulmonary edema.
-
Treatment of underlying infection (e.g., antibiotics for pneumonia): Targeting the root cause of the problem is crucial.
-
Supportive care: Includes monitoring vital signs, fluid balance, and electrolyte levels.
Conclusion:
The simultaneous occurrence of pulmonary edema and impaired ventilation represents a critical medical condition requiring prompt diagnosis and treatment. Understanding the underlying mechanisms and clinical manifestations is crucial for effective management. The interaction between these two conditions significantly impacts patient prognosis, highlighting the importance of early intervention and comprehensive supportive care. Further research continues to refine diagnostic and therapeutic approaches, ultimately improving outcomes for individuals experiencing this life-threatening combination of respiratory and cardiovascular compromise. This detailed overview serves as a starting point for a deeper understanding of this complex interplay of pathophysiological processes.
Latest Posts
Latest Posts
-
Which Information Is Often Not Included In A Bank Statement
Apr 02, 2025
-
Health Care Providers Who Infrequently Work Together
Apr 02, 2025
-
The Remains Of Doctor Bass Answer Key
Apr 02, 2025
-
Similarities Between French Revolution And American Revolution
Apr 02, 2025
-
Becoming A Professional Nurse Professional Behaviors In Nursing
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Pulmonary Edema And Impaired Ventilation Occur During: . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
