Reassessment Of A Patient With A Medical Complaint
Breaking News Today
Mar 30, 2025 · 6 min read
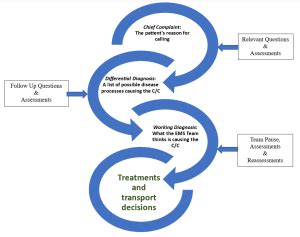
Table of Contents
Reassessment of a Patient with a Medical Complaint: A Comprehensive Guide
Reassessing a patient's condition is a cornerstone of effective healthcare. It's not simply a repeat of the initial assessment; rather, it's a dynamic process that involves critically evaluating the patient's response to treatment, identifying any changes in their condition, and adapting the care plan accordingly. This comprehensive guide delves into the intricacies of patient reassessment, providing a framework for healthcare professionals to deliver optimal patient care.
Understanding the Importance of Reassessment
Regular reassessment is crucial for several reasons:
Early Detection of Complications:
A timely reassessment can detect complications early, allowing for prompt intervention and potentially preventing serious adverse outcomes. Changes in vital signs, pain levels, or mental status can signal developing complications like infection, hemorrhage, or organ dysfunction. Early detection is key to effective management and improved patient outcomes.
Monitoring Treatment Effectiveness:
Reassessment helps determine whether the chosen treatment is effective. If a patient's condition doesn't improve or worsens despite treatment, reassessment allows for a reevaluation of the diagnosis, treatment plan, or underlying causes. This iterative process is essential for personalized and effective medicine.
Identifying New or Changing Symptoms:
Patients may experience new symptoms or a change in existing symptoms that weren't initially apparent. Reassessment provides an opportunity to uncover these changes, leading to adjustments in the care plan to address the evolving needs of the patient. This highlights the importance of open communication and patient-centered care.
Adjusting the Care Plan:
Based on the findings of the reassessment, the healthcare professional can adjust the care plan accordingly. This may involve modifying medication dosages, adding new interventions, or changing the treatment approach altogether. Flexibility and adaptability are essential elements of effective patient management.
Enhancing Patient Satisfaction:
Regular reassessment demonstrates the healthcare professional's commitment to the patient's well-being. It reassures the patient that their concerns are being heard and addressed, fostering trust and improving overall patient satisfaction. This patient-centered approach is vital for building positive therapeutic relationships.
The Reassessment Process: A Step-by-Step Approach
The reassessment process is not a rigid formula; it adapts to the specific needs of each patient and their presenting complaint. However, a structured approach can ensure a thorough and effective evaluation.
1. Review the Initial Assessment:
Begin by thoroughly reviewing the patient's initial assessment, including their medical history, presenting complaint, initial vital signs, physical examination findings, diagnostic test results, and the initial treatment plan. This provides a baseline for comparison and helps identify any deviations from the expected trajectory.
2. Gather Subjective Data:
Engage in a conversation with the patient, focusing on the following:
- Current Symptoms: Ask about any changes in their existing symptoms, the intensity, frequency, and duration of these symptoms, and the presence of any new symptoms. Use open-ended questions to encourage detailed responses. Active listening is crucial during this phase.
- Pain Assessment: If pain is present, reassess its location, intensity (using a pain scale), quality (e.g., sharp, dull, aching), duration, and any aggravating or relieving factors. Use standardized pain assessment tools when appropriate.
- Medication Effects: Inquire about the effectiveness of any prescribed medications, including any side effects experienced. This is essential for medication management and patient safety.
- Emotional State: Assess the patient's emotional well-being, noting any signs of anxiety, depression, or distress. Addressing emotional needs is a vital component of holistic care.
- Compliance with Treatment: Determine the patient's adherence to the prescribed treatment plan. Identifying barriers to compliance is crucial for improving treatment outcomes.
3. Gather Objective Data:
Conduct a physical examination, focusing on the areas relevant to the patient's presenting complaint. This might include:
- Vital Signs: Reassess vital signs (temperature, heart rate, respiratory rate, blood pressure, oxygen saturation) and compare them to the initial readings. Significant changes warrant further investigation.
- Neurological Assessment: If indicated, assess neurological function, including level of consciousness, orientation, motor strength, and reflexes. This is crucial for detecting neurological complications.
- Cardiovascular Assessment: Auscultate the heart and lungs, noting any abnormalities like murmurs, rales, or wheezes. Cardiovascular assessment is particularly important in patients with cardiac conditions.
- Respiratory Assessment: Assess respiratory effort, breath sounds, and oxygen saturation. Respiratory reassessment is essential in patients with respiratory problems.
- Gastrointestinal Assessment: Assess abdominal distension, bowel sounds, and tenderness. This is important for detecting gastrointestinal complications.
- Wound Assessment (if applicable): Assess the appearance, size, and drainage of any wounds. Wound assessment is crucial for preventing infection and promoting healing.
- Review of Diagnostic Tests: Review any new or repeated diagnostic test results. These results provide objective data to inform clinical decision-making.
4. Analyze and Interpret Data:
Integrate the subjective and objective data to form a comprehensive picture of the patient's current condition. Compare the findings with the initial assessment to identify any significant changes. Critical thinking and clinical judgment are essential at this stage.
5. Modify the Care Plan:
Based on your analysis, adjust the care plan as needed. This may involve:
- Changing Medications: Adjusting dosages, adding new medications, or discontinuing existing ones.
- Adding New Interventions: Implementing new treatments, such as physiotherapy, respiratory therapy, or wound care.
- Referring to Specialists: Consulting with specialists for further evaluation or management.
- Altering the Discharge Plan: Modifying the discharge plan based on the patient's progress and needs.
6. Document Thoroughly:
Meticulously document all aspects of the reassessment, including the subjective and objective findings, your analysis, and any modifications made to the care plan. Clear and concise documentation is essential for continuity of care and legal protection.
Common Scenarios Requiring Reassessment
Reassessment is necessary in a wide range of clinical situations. Here are some common scenarios:
- Post-surgical patients: Regular reassessment is crucial to detect potential complications like infection, hemorrhage, or deep vein thrombosis.
- Patients with acute conditions: Patients with conditions like pneumonia, heart failure, or stroke require frequent reassessment to monitor their response to treatment and detect any deterioration.
- Patients receiving intravenous fluids or medications: Close monitoring is needed to detect adverse reactions and ensure fluid balance.
- Patients with chronic conditions: Regular reassessment is essential for managing chronic conditions like diabetes, hypertension, and asthma.
- Patients experiencing changes in symptoms: Any new or worsening symptoms warrant a prompt reassessment.
Challenges in Reassessment and Strategies for Improvement
Several challenges can complicate the reassessment process:
- Time constraints: Healthcare professionals often face time pressures, which can limit the thoroughness of the reassessment. Effective time management and prioritization are crucial.
- Communication barriers: Language barriers, cognitive impairment, or hearing difficulties can hinder effective communication with the patient. Utilizing interpreters, communication aids, and patience are essential.
- Subjectivity of symptoms: Patients may describe their symptoms differently, making it challenging to accurately assess their condition. Using standardized assessment tools and open-ended questions can mitigate this challenge.
- Lack of resources: Limited access to diagnostic testing or specialized personnel can hinder the effectiveness of the reassessment. Advocating for resources and utilizing available technology can help overcome this limitation.
Conclusion
Reassessment is a dynamic and crucial component of providing high-quality patient care. By employing a structured approach, engaging in open communication with the patient, and utilizing critical thinking skills, healthcare professionals can effectively identify changes in the patient's condition, adjust the care plan, and ultimately improve patient outcomes. The commitment to regular and thorough reassessment signifies a dedication to patient-centered care and reflects the evolving nature of healthcare. Continued professional development and a focus on best practices are essential for mastering the art of patient reassessment and delivering the highest standard of care.
Latest Posts
Latest Posts
-
Which Statement Best Defines An Automatic Call Distribution System
Apr 01, 2025
-
Which Statement Best Describes The Satire In The Excerpt
Apr 01, 2025
-
Jobs For Entry Level Beauty And Wellness Professionals
Apr 01, 2025
-
When Is An Ifr Flight Plan Required
Apr 01, 2025
-
Incoming Solar Flux Values From January To December 2003
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Reassessment Of A Patient With A Medical Complaint . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
