Rn Alterations In Cardiovascular Function And Perfusion Assessment
Breaking News Today
Mar 19, 2025 · 6 min read
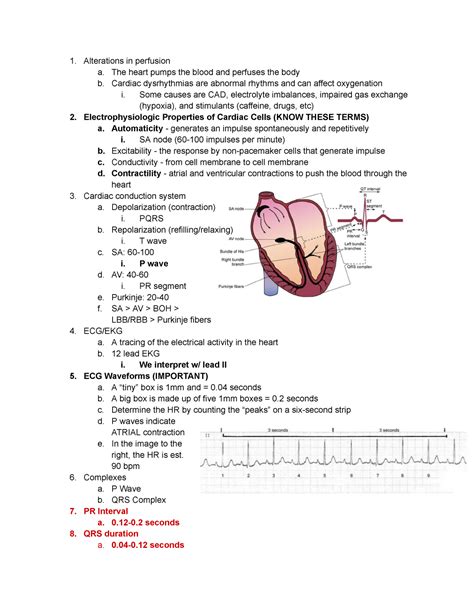
Table of Contents
RN Alterations in Cardiovascular Function and Perfusion Assessment: A Comprehensive Guide
Registered nurses (RNs) play a crucial role in assessing and managing alterations in cardiovascular function and perfusion. This comprehensive guide delves into the complexities of cardiovascular physiology, common alterations, and the essential assessment techniques RNs employ to ensure optimal patient care. We will explore various conditions, diagnostic tools, and nursing interventions, all crucial for providing safe and effective care to patients with compromised cardiovascular health.
Understanding Cardiovascular Physiology: The Foundation of Assessment
Before diving into alterations, a solid understanding of normal cardiovascular function is paramount. The cardiovascular system, comprised of the heart and blood vessels, is responsible for delivering oxygen and nutrients to the body's tissues while removing waste products. This intricate process relies on efficient:
1. Cardiac Output (CO):
The volume of blood pumped by the heart per minute. CO is a critical indicator of overall cardiovascular performance and is influenced by heart rate (HR) and stroke volume (SV). Understanding the interplay between HR and SV is essential for interpreting changes in CO.
2. Stroke Volume (SV):
The amount of blood ejected from the left ventricle with each contraction. SV is determined by preload, afterload, and contractility.
- Preload: The volume of blood in the ventricles at the end of diastole (relaxation). Increased preload typically leads to increased SV, up to a point.
- Afterload: The resistance the left ventricle must overcome to eject blood into the aorta. Increased afterload reduces SV.
- Contractility: The force of ventricular contraction. Enhanced contractility increases SV.
3. Systemic Vascular Resistance (SVR):
The resistance to blood flow in the arteries. High SVR indicates vasoconstriction, while low SVR suggests vasodilation. SVR significantly impacts blood pressure.
4. Blood Pressure (BP):
The force exerted by blood against the arterial walls. BP is influenced by CO and SVR. Maintaining adequate BP is crucial for tissue perfusion.
Common Alterations in Cardiovascular Function: Recognizing the Signs
Numerous conditions can disrupt the delicate balance of the cardiovascular system. RNs must be adept at recognizing the subtle and overt signs of these alterations.
1. Heart Failure (HF):
A complex clinical syndrome characterized by the heart's inability to pump enough blood to meet the body's metabolic demands. HF can be categorized as systolic (reduced ejection fraction) or diastolic (impaired ventricular relaxation). Common symptoms include dyspnea, fatigue, edema, and orthopnea.
2. Coronary Artery Disease (CAD):
Narrowing of the coronary arteries, reducing blood flow to the heart muscle. CAD can lead to angina pectoris (chest pain), myocardial infarction (heart attack), and ultimately, heart failure. Risk factors include hypertension, hyperlipidemia, smoking, and diabetes.
3. Arrhythmias:
Abnormal heart rhythms, which can range from benign to life-threatening. Arrhythmias can affect heart rate, rhythm, and the efficiency of blood pumping. Symptoms vary depending on the type and severity of the arrhythmia and may include palpitations, dizziness, and syncope.
4. Hypertension (HTN):
Persistently elevated blood pressure, placing increased strain on the cardiovascular system. Untreated HTN increases the risk of CAD, HF, stroke, and renal failure. Often asymptomatic in the early stages, HTN requires regular monitoring and management.
5. Hypotension:
Abnormally low blood pressure, insufficient to perfuse vital organs. Hypotension can be caused by various factors, including dehydration, hemorrhage, and sepsis. Symptoms may include dizziness, lightheadedness, and fainting.
6. Shock:
A life-threatening condition characterized by inadequate tissue perfusion. Different types of shock exist, including cardiogenic (pump failure), hypovolemic (fluid loss), septic (infection), and anaphylactic (allergic reaction). Early recognition and aggressive treatment are crucial for survival.
Perfusion Assessment: The RN's Vital Role
Accurate and timely assessment of perfusion is critical in identifying and managing cardiovascular alterations. RNs utilize a range of techniques to assess perfusion, including:
1. Vital Signs:
Regular monitoring of heart rate, blood pressure, respiratory rate, and temperature provides crucial baseline data and allows for early detection of changes. Tachycardia, hypotension, and tachypnea can indicate compromised perfusion.
2. Physical Assessment:
A comprehensive physical exam includes:
- Skin assessment: Assessing skin color, temperature, moisture, and capillary refill time. Pale, cool, clammy skin, and prolonged capillary refill time suggest poor perfusion.
- Heart sounds: Auscultating for heart murmurs, extra heart sounds, and changes in heart rate and rhythm.
- Lung sounds: Assessing for crackles, wheezes, and diminished breath sounds, indicative of fluid overload or pulmonary edema.
- Peripheral pulses: Palpating peripheral pulses to assess strength and symmetry. Weak or absent pulses indicate decreased perfusion to the extremities.
- Edema: Assessing for swelling in the extremities, which can indicate fluid overload or venous insufficiency.
3. Diagnostic Testing:
RNs play a vital role in assisting with and monitoring patients undergoing diagnostic tests, including:
- Electrocardiogram (ECG): Provides information about heart rhythm and electrical activity.
- Echocardiogram: Uses ultrasound to visualize heart structures and assess function.
- Cardiac catheterization: A more invasive procedure used to visualize coronary arteries and assess for blockages.
- Blood tests: Including cardiac enzymes (e.g., troponin), electrolytes, and blood counts, to assess heart damage and overall health.
Nursing Interventions: Optimizing Cardiovascular Function and Perfusion
Based on the assessment findings, RNs implement various interventions to support cardiovascular function and improve perfusion. These interventions may include:
1. Medications:
Administering medications as prescribed, including:
- Cardiac glycosides (e.g., digoxin): Improve cardiac contractility.
- Beta-blockers: Reduce heart rate and blood pressure.
- ACE inhibitors: Reduce blood pressure and afterload.
- Diuretics: Reduce fluid overload.
- Vasodilators: Dilate blood vessels to reduce blood pressure and improve perfusion.
- Anticoagulants: Prevent blood clot formation.
2. Fluid Management:
Managing fluid balance is crucial for maintaining adequate blood volume and perfusion. This involves monitoring fluid intake and output, administering intravenous fluids as needed, and adjusting medication regimens as necessary.
3. Oxygen Therapy:
Providing supplemental oxygen to increase oxygen saturation and improve tissue perfusion.
4. Monitoring:
Continuous monitoring of vital signs, cardiac rhythm, and oxygen saturation is essential to detect any deterioration in cardiovascular status.
5. Patient Education:
Educating patients about their condition, medication regimen, lifestyle modifications (e.g., diet, exercise, smoking cessation), and warning signs of deterioration is vital for long-term management and improved outcomes.
6. Psychological Support:
Providing emotional support and addressing psychological concerns associated with cardiovascular conditions is crucial for patient well-being.
Conclusion: The Ongoing Role of the RN in Cardiovascular Care
The assessment and management of alterations in cardiovascular function and perfusion are complex and require a high level of skill and knowledge. Registered nurses play a pivotal role in this process, from conducting thorough assessments to implementing appropriate interventions and educating patients. Continuous learning and staying abreast of the latest advancements in cardiovascular care are vital to ensure the delivery of high-quality, patient-centered care. The information presented here provides a foundational understanding, and further specialized education is essential for RNs working in cardiology or critical care settings. The ultimate goal is to improve patient outcomes by optimizing cardiovascular function and maintaining adequate tissue perfusion.
Latest Posts
Latest Posts
-
Refers To A Seat In Congress Without An Incumbent
Mar 19, 2025
-
Study Of The Organization And Operation Of Governments
Mar 19, 2025
-
The Supreme Court Has Decided That The Death Penalty
Mar 19, 2025
-
An Applicant Who Receives A Preferred Risk Classification Qualifies For
Mar 19, 2025
-
Write 61 80 As A Decimal Number
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Rn Alterations In Cardiovascular Function And Perfusion Assessment . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
