Sickle Cell Disease Is Caused By Quizlet
Breaking News Today
Mar 23, 2025 · 6 min read
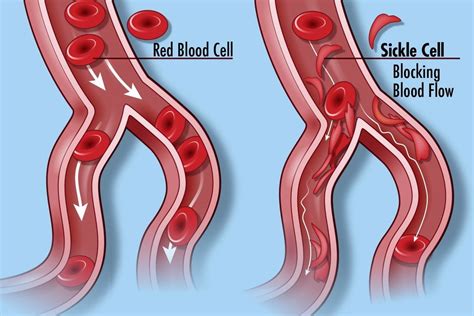
Table of Contents
Sickle Cell Disease: A Comprehensive Overview
Sickle cell disease (SCD) is a serious inherited blood disorder that affects millions worldwide. Understanding its causes, symptoms, and management is crucial for effective prevention and treatment. This in-depth article explores the genetic basis of SCD, its pathophysiology, clinical manifestations, and current treatment approaches.
What Causes Sickle Cell Disease?
At the heart of SCD lies a genetic mutation affecting the gene responsible for producing hemoglobin, the protein in red blood cells that carries oxygen throughout the body. Hemoglobin is comprised of four subunits: two alpha-globin chains and two beta-globin chains. In individuals with SCD, a single point mutation in the beta-globin gene leads to the production of abnormal hemoglobin, known as hemoglobin S (HbS).
The Genetic Mutation: A Closer Look
This specific mutation involves a single nucleotide substitution, changing the amino acid glutamic acid to valine at the sixth position of the beta-globin chain. This seemingly small change has profound consequences. Normal hemoglobin (hemoglobin A, or HbA) is flexible and easily traverses blood vessels. However, HbS polymerizes under low-oxygen conditions, forming rigid, rod-like structures that distort the shape of red blood cells. These abnormally shaped cells, known as sickle cells, are less flexible and prone to getting stuck in small blood vessels, causing blockages.
Inheritance Patterns: Autosomal Recessive Inheritance
SCD is inherited in an autosomal recessive manner. This means that an individual must inherit two copies of the mutated beta-globin gene – one from each parent – to develop the disease. Individuals who inherit only one copy of the mutated gene are carriers, exhibiting sickle cell trait (SCT). While carriers typically do not experience the severe symptoms of SCD, they can still pass the mutated gene to their offspring.
- Homozygous SCD: Individuals with two copies of the mutated gene (HbS/HbS) have SCD.
- Heterozygous SCT: Individuals with one copy of the mutated gene and one copy of the normal gene (HbA/HbS) have SCT.
Understanding the Risk of Inheritance
The likelihood of a child inheriting SCD depends on the parents' genotypes. If both parents have SCT, there's a 25% chance their child will inherit two copies of the mutated gene and develop SCD, a 50% chance the child will inherit one mutated gene and have SCT, and a 25% chance the child will inherit two normal genes and be unaffected. Genetic counseling can help prospective parents understand their risk of having a child with SCD.
Pathophysiology of Sickle Cell Disease: The Molecular Mechanism
The hallmark of SCD is the sickling of red blood cells. This process is triggered by deoxygenation. When oxygen levels are low, HbS molecules aggregate, forming long fibers that deform the red blood cells into their characteristic sickle shape. These sickled cells are less flexible and more prone to hemolysis (destruction). Their rigidity causes them to obstruct blood flow, leading to a variety of complications.
Vaso-occlusive Crises: The Core Problem
The most common complication of SCD is the vaso-occlusive crisis (VOC). VOCs occur when sickled red blood cells obstruct blood flow in small blood vessels. This blockage deprives tissues and organs of oxygen and nutrients, leading to intense pain, inflammation, and organ damage. The location and severity of VOCs vary widely, affecting different parts of the body.
Hemolysis and Anemia
The destruction of sickled red blood cells leads to hemolytic anemia. This means the body doesn't produce enough healthy red blood cells to carry sufficient oxygen throughout the body, resulting in fatigue, weakness, shortness of breath, and pallor. The chronic hemolysis also contributes to other complications.
Other Complications of Sickle Cell Disease
The chronic nature of SCD and its various pathophysiological mechanisms lead to a wide range of complications, including:
- Acute Chest Syndrome (ACS): A life-threatening complication characterized by lung inflammation and infection.
- Stroke: Blockage of blood vessels in the brain leading to neurological damage.
- Splenic Sequestration: Accumulation of sickled cells in the spleen, potentially leading to splenic enlargement and rupture.
- Retinopathy: Damage to the blood vessels in the eyes, potentially causing vision impairment.
- Chronic Organ Damage: Repeated VOCs and chronic hemolysis can lead to long-term damage to various organs, including the kidneys, liver, heart, and lungs.
- Infection: Individuals with SCD are more susceptible to infections due to functional asplenia (reduced spleen function) and impaired immune response.
Clinical Manifestations of Sickle Cell Disease
The symptoms of SCD vary significantly among individuals, ranging in severity and frequency. Some individuals experience relatively mild symptoms, while others face frequent and severe complications. The onset of symptoms can occur in infancy or later in life.
Common Symptoms:
- Pain: The most common symptom, ranging from mild to excruciating pain during VOCs. The pain can affect various parts of the body, including bones, joints, abdomen, chest, and extremities.
- Fatigue: Due to anemia, resulting in decreased energy levels.
- Shortness of breath: Caused by anemia and reduced oxygen-carrying capacity.
- Pallor: Pale skin color due to low red blood cell count.
- Jaundice: Yellowing of the skin and eyes due to excessive breakdown of red blood cells.
- Hand-foot syndrome: Swelling of the hands and feet in infants.
- Priapism: Persistent and painful erection in males.
Severe Complications:
As mentioned previously, severe complications include ACS, stroke, splenic sequestration, retinopathy, and chronic organ damage. These complications require prompt medical attention and can be life-threatening.
Diagnosis and Management of Sickle Cell Disease
Early diagnosis is crucial for effective management of SCD. Diagnosis typically involves:
- Newborn screening: Most developed countries perform newborn screening for SCD, allowing for early intervention.
- Hemoglobin electrophoresis: A blood test that identifies the different types of hemoglobin present in the blood, confirming the presence of HbS.
- Genetic testing: Confirms the presence of the specific gene mutation responsible for SCD.
Treatment Strategies for Sickle Cell Disease
Managing SCD involves a multifaceted approach aimed at reducing the frequency and severity of VOCs, preventing complications, and improving the overall quality of life.
Pain Management
Effective pain management is a cornerstone of SCD care. This often includes:
- Analgesics: Pain medications such as opioids, NSAIDs, and acetaminophen.
- Hydration: Maintaining adequate fluid intake helps to improve blood flow and reduce sickling.
- Oxygen therapy: Increases oxygen levels in the blood to reduce sickling.
Hydroxyurea
Hydroxyurea is a medication that increases the production of fetal hemoglobin (HbF), a type of hemoglobin that doesn't sickle. HbF can reduce the severity of SCD symptoms.
Blood Transfusions
Regular blood transfusions can help improve oxygen-carrying capacity and reduce the frequency of VOCs. However, chronic transfusions can lead to iron overload, requiring chelation therapy.
Bone Marrow Transplant
Bone marrow transplantation (BMT) is a potentially curative treatment for SCD, but it is associated with significant risks and is not suitable for all individuals.
Gene Therapy
Gene therapy approaches are currently under development and hold promise for providing a potential cure for SCD. These strategies aim to correct the underlying genetic defect responsible for HbS production.
Conclusion: Living with Sickle Cell Disease
Sickle cell disease is a complex and challenging condition that requires ongoing medical care. While a cure is not yet available for all individuals, advancements in treatment strategies continue to improve the lives of those affected by this disease. Early diagnosis, proactive management, and access to comprehensive healthcare services are essential for improving the overall health and well-being of individuals with SCD. Ongoing research continues to explore new and innovative therapies with the ultimate goal of finding a cure and significantly reducing the burden of this disease. The information provided here is intended for educational purposes and should not replace advice from a healthcare professional.
Latest Posts
Latest Posts
-
Which Of The Following Best Describes Dating Violence
Mar 24, 2025
-
Which Of The Following Are Correctly Matched
Mar 24, 2025
-
Volume Is The Amount Of What In An Object
Mar 24, 2025
-
Hyperventilation Could Be Associated With All Of The Following Except
Mar 24, 2025
-
Virex Tb And Cavi Wipes Are Used For What Purpose
Mar 24, 2025
Related Post
Thank you for visiting our website which covers about Sickle Cell Disease Is Caused By Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
