Signs Of A Pulmonary Blast Injury Include
Breaking News Today
Mar 15, 2025 · 7 min read
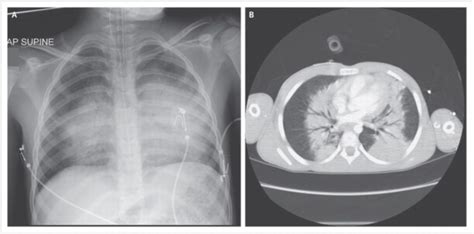
Table of Contents
Signs of a Pulmonary Blast Injury: Recognizing and Responding to a Life-Threatening Condition
Pulmonary blast injury (PBI) is a devastating and often overlooked consequence of explosions. Unlike primary blast injuries (direct damage from the blast wave to organs), PBI results from the interaction of the blast wave with the lungs and the subsequent cascade of physiological effects. Recognizing the signs of PBI is crucial for timely intervention and improved patient outcomes, as this condition can rapidly progress and become life-threatening. This article will delve into the various signs and symptoms of PBI, covering both immediate and delayed manifestations, as well as the underlying pathophysiology that drives these clinical presentations.
Understanding the Pathophysiology of Pulmonary Blast Injury
To understand the signs and symptoms of PBI, it's essential to grasp the underlying mechanisms. An explosion generates a shockwave that travels through the air, impacting the lungs directly and indirectly. The direct effects involve the immediate compression and expansion of lung tissue, causing shearing forces that damage alveoli (tiny air sacs in the lungs) and blood vessels. This can lead to:
Direct Lung Damage:
- Alveolar rupture and hemorrhage: The forceful pressure changes can rupture fragile alveoli, leading to bleeding into the lungs (pulmonary hemorrhage). This bleeding can manifest as hemoptysis (coughing up blood).
- Pulmonary contusion: Blunt trauma to the lungs from the blast wave can cause bruising and bleeding within the lung tissue. This can impair gas exchange and lead to respiratory distress.
- Capillary damage: The sheer forces can damage the delicate capillaries in the lungs, leading to increased permeability and fluid leakage into the alveoli. This fluid accumulation further hinders gas exchange.
Indirect Lung Damage:
The indirect effects of the blast wave are just as significant. The initial wave creates a pressure differential, causing barotrauma (pressure-related injury) within the respiratory system. This can trigger a cascade of events:
- Airway obstruction: The force of the blast can cause airway swelling, narrowing, and even complete obstruction, leading to hypoxia (lack of oxygen).
- Pneumothorax: The pressure differential can cause air to leak into the pleural space (the space between the lung and chest wall), collapsing the lung (pneumothorax). This is a life-threatening condition that requires immediate medical attention.
- Hemothorax: Similar to pneumothorax, the pressure changes can cause blood to accumulate in the pleural space (hemothorax), further compromising lung function.
- Pulmonary edema: Increased capillary permeability leads to fluid accumulation in the alveoli, causing pulmonary edema. This compromises gas exchange and leads to severe respiratory distress.
- ARDS (Acute Respiratory Distress Syndrome): In severe cases, PBI can progress to ARDS, a life-threatening condition characterized by widespread inflammation and fluid accumulation in the lungs.
Immediate Signs and Symptoms of Pulmonary Blast Injury
The signs and symptoms of PBI can vary widely depending on the severity of the blast exposure. Immediate symptoms usually appear within the first few hours after the blast:
Respiratory Symptoms:
- Dyspnea (shortness of breath): This is a hallmark symptom of PBI and often presents immediately after the blast. The severity can range from mild breathlessness to severe respiratory distress.
- Cough: A persistent cough, sometimes productive of blood (hemoptysis), is a common finding.
- Wheezing: Airway obstruction can cause wheezing sounds during breathing.
- Tachypnea (rapid breathing): The body attempts to compensate for reduced oxygen levels by increasing the breathing rate.
- Cyanosis (bluish discoloration of the skin): This indicates inadequate oxygenation of the blood.
- Hypoxia (low blood oxygen levels): This is a serious complication and can be detected using pulse oximetry.
Other Symptoms:
- Chest pain: Pain in the chest is often present, especially with pulmonary contusions or pneumothorax.
- Hemoptysis (coughing up blood): This indicates alveolar damage and bleeding within the lungs.
- Hypotension (low blood pressure): This can result from blood loss due to pulmonary hemorrhage or other associated injuries.
- Tachycardia (rapid heart rate): The body compensates for hypoxia and blood loss by increasing the heart rate.
- Altered mental status: Hypoxia can impair brain function, leading to confusion, disorientation, or loss of consciousness.
Delayed Signs and Symptoms of Pulmonary Blast Injury
While some symptoms appear immediately, others may not manifest for hours, days, or even weeks after the blast event. These delayed symptoms are often due to the ongoing inflammatory response and the development of complications:
Progressive Respiratory Distress:
- Worsening dyspnea: Shortness of breath can progressively worsen as pulmonary edema and ARDS develop.
- Increased oxygen requirement: Patients may require increasing levels of supplemental oxygen to maintain adequate blood oxygenation.
- Development of ARDS: This life-threatening condition is characterized by severe hypoxemia (low blood oxygen levels), respiratory failure, and the need for mechanical ventilation.
Other Delayed Manifestations:
- Infection: Damage to the lungs increases the risk of pneumonia and other respiratory infections.
- Multi-organ failure: Severe PBI can lead to failure of other organs, such as the kidneys and heart, due to hypoxia and systemic inflammation.
- Psychological trauma: The experience of a blast event can lead to significant psychological distress, including post-traumatic stress disorder (PTSD).
Diagnosing Pulmonary Blast Injury
Diagnosing PBI involves a combination of clinical evaluation, imaging studies, and blood tests:
- Physical examination: Careful assessment of respiratory rate, oxygen saturation, heart rate, and blood pressure is crucial. Auscultation (listening to the lungs) may reveal abnormal breath sounds, such as wheezes or crackles.
- Chest X-ray: This is the initial imaging study used to detect pneumothorax, hemothorax, pulmonary contusions, and pulmonary edema.
- CT scan: A CT scan provides more detailed images of the lungs and can help identify subtle injuries not visible on a chest X-ray.
- Arterial blood gas analysis: This test measures the levels of oxygen and carbon dioxide in the blood, providing crucial information about the severity of hypoxia and respiratory impairment.
- Complete blood count (CBC): This helps assess for anemia (low red blood cell count) due to blood loss.
Management of Pulmonary Blast Injury
The management of PBI is complex and requires a multidisciplinary approach. Treatment focuses on supporting respiratory function, managing complications, and providing supportive care:
- Oxygen therapy: Supplemental oxygen is essential to correct hypoxia.
- Mechanical ventilation: Patients with severe respiratory distress may require mechanical ventilation to support breathing.
- Fluid management: Careful fluid management is crucial to prevent both dehydration and fluid overload.
- Treatment of pneumothorax and hemothorax: These conditions often require chest tube insertion to drain air or blood from the pleural space.
- Antibiotics: Antibiotics may be necessary to prevent or treat respiratory infections.
- Pain management: Analgesics (pain relievers) are used to manage chest pain.
- Supportive care: This includes nutritional support, monitoring for complications, and addressing psychological trauma.
Prognosis and Long-Term Effects
The prognosis for PBI varies significantly depending on the severity of the injury and the availability of prompt and effective medical care. Early recognition and treatment are crucial for improving patient outcomes. Even with appropriate treatment, some individuals may experience long-term effects, including:
- Chronic respiratory problems: Some patients may experience persistent shortness of breath, cough, and decreased lung function.
- Post-traumatic stress disorder (PTSD): The emotional impact of a blast injury can lead to PTSD, requiring psychological support.
- Reduced quality of life: The long-term effects of PBI can significantly impact an individual's quality of life, affecting their ability to work, exercise, and participate in social activities.
Conclusion
Pulmonary blast injury is a serious and potentially life-threatening condition that requires prompt recognition and treatment. Understanding the various signs and symptoms, both immediate and delayed, is crucial for healthcare professionals involved in the care of blast injury victims. Early intervention, including supportive respiratory care and management of complications, is essential for improving patient outcomes and minimizing long-term effects. Further research into the pathophysiology and treatment of PBI is crucial to enhance our understanding of this complex condition and ultimately improve the lives of those affected. The information provided in this article is for educational purposes only and should not be considered medical advice. Always seek the guidance of a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Latest Posts
Latest Posts
-
Administrative Civil Or Criminal Sanctions Cui Quizlet
Mar 18, 2025
-
Sinners In The Hands Of An Angry God Quizlet
Mar 18, 2025
-
Lord Of The Flies Chapter 7 Quizlet
Mar 18, 2025
-
John Receives An Email About A Potential Shutdown Quizlet
Mar 18, 2025
-
A License To Practice Medicine Is Quizlet
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Signs Of A Pulmonary Blast Injury Include . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
