Symptomatic Hypoglycemia Will Most Likely Develop If A Patient
Breaking News Today
Mar 15, 2025 · 6 min read
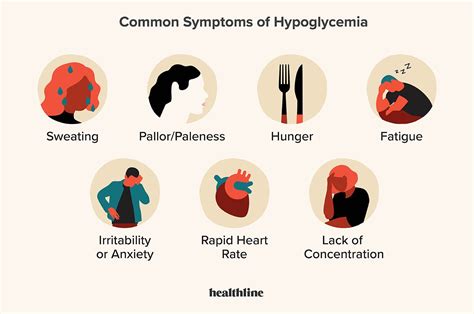
Table of Contents
Symptomatic Hypoglycemia: Who's Most at Risk?
Symptomatic hypoglycemia, or low blood sugar with noticeable symptoms, is a serious condition that can significantly impact a person's quality of life. Understanding who is most likely to develop this condition is crucial for preventative measures and effective management. This article delves deep into the risk factors, exploring the underlying causes and highlighting the patient profiles most susceptible to experiencing symptomatic hypoglycemia.
Understanding Hypoglycemia
Before we dive into the risk factors, let's establish a clear understanding of hypoglycemia itself. Hypoglycemia occurs when your blood glucose (blood sugar) levels drop too low. The body needs glucose for energy, and when levels fall below a certain threshold (generally considered to be below 70 mg/dL), various symptoms can manifest. These symptoms vary in severity and can range from mild discomfort to life-threatening complications. It's crucial to differentiate between asymptomatic hypoglycemia (where symptoms are absent) and symptomatic hypoglycemia (where symptoms are present and noticeable). This article focuses primarily on symptomatic hypoglycemia.
Who is Most Likely to Develop Symptomatic Hypoglycemia?
Several factors increase the likelihood of developing symptomatic hypoglycemia. These factors often interact, creating a complex interplay of risk. Let's break down the key patient profiles:
1. Patients with Diabetes Mellitus
This is perhaps the most significant risk factor. Both type 1 and type 2 diabetes can lead to hypoglycemia, although the mechanisms differ.
-
Type 1 Diabetes: Individuals with type 1 diabetes rely on insulin injections or insulin pumps to manage their blood sugar levels. Taking too much insulin, skipping meals, or engaging in strenuous physical activity without adjusting insulin dosage can easily trigger hypoglycemia. The precise insulin dose required can vary based on several factors including food intake, activity level and individual response to treatment.
-
Type 2 Diabetes: While less common than in type 1 diabetes, hypoglycemia can occur in type 2 diabetes, especially in those using insulin or certain oral medications (like sulfonylureas) that stimulate insulin release. These medications can cause excessive insulin secretion, leading to a drop in blood glucose. Additionally, patients with type 2 diabetes may have impaired glucose counter-regulation mechanisms making them more susceptible to severe hypoglycemic episodes.
Key Consideration: Patients with diabetes who are elderly or have impaired awareness of hypoglycemic symptoms are at a particularly high risk of severe or silent hypoglycemia.
2. Patients on Certain Medications
Beyond diabetes medications, several other drugs can contribute to hypoglycemia:
-
Sulfonylureas: As mentioned above, these oral antidiabetic medications increase insulin release, potentially leading to hypoglycemia, especially if combined with inadequate food intake or missed meals.
-
Meglitinides: Similar to sulfonylureas, meglitinides stimulate insulin secretion and can cause hypoglycemia.
-
Salicylates (Aspirin): High doses of aspirin can increase insulin sensitivity and potentially contribute to hypoglycemia in susceptible individuals.
-
Beta-blockers: These medications can mask the symptoms of hypoglycemia, making it harder for individuals to recognize and treat low blood sugar. This is because beta-blockers inhibit the body's natural response to hypoglycemia which includes an increased heart rate and tremor.
-
Alcohol: Alcohol consumption can interfere with gluconeogenesis (the liver's production of glucose) and increase insulin sensitivity, leading to hypoglycemia, particularly when consumed on an empty stomach.
3. Patients with Impaired Glucose Counter-Regulation
Glucose counter-regulation is the body's natural response to low blood sugar. This involves several hormonal and metabolic processes designed to raise blood glucose levels. Impaired counter-regulation means these processes are not functioning optimally, increasing the risk of hypoglycemia. This impairment is often seen in:
-
Individuals with long-standing diabetes: Prolonged periods of hyperglycemia can damage the mechanisms responsible for counter-regulation.
-
Patients with certain endocrine disorders: Conditions affecting the adrenal glands, pituitary gland, or pancreas can disrupt the hormonal signals involved in glucose regulation.
-
Patients with severe liver disease: The liver plays a vital role in glucose production. Liver impairment compromises this function, making individuals more prone to hypoglycemia.
4. Patients with Malnutrition or Eating Disorders
Individuals who are malnourished or have eating disorders like anorexia nervosa or bulimia nervosa are at a significantly increased risk of hypoglycemia. Inadequate calorie intake and nutrient deficiencies compromise the body's ability to maintain stable blood glucose levels. This is exacerbated by the unpredictable nature of eating patterns associated with eating disorders.
5. Patients with Insulinoma
An insulinoma is a rare tumor of the pancreas that produces excessive insulin. This leads to persistent hypoglycemia, often requiring surgical removal of the tumor for successful management. These individuals may experience hypoglycemic symptoms even after meals.
6. Patients with Critical Illness or Sepsis
Severe illness and sepsis can significantly impact glucose metabolism. The body's stress response and inflammatory processes can lead to both hyperglycemia (high blood sugar) and hypoglycemia. The risk of hypoglycemia is particularly increased during periods of starvation or inadequate nutritional support in critically ill patients.
7. Patients with Genetic Disorders
Rare genetic disorders affecting glucose metabolism can predispose individuals to hypoglycemia. These disorders often involve defects in enzymes crucial for glucose production or utilization.
Recognizing the Symptoms of Symptomatic Hypoglycemia
Recognizing the symptoms of hypoglycemia is crucial for prompt treatment. Symptoms can vary from person to person but commonly include:
-
Neuroglycopenic Symptoms: These symptoms are caused by the brain's lack of glucose and can include confusion, dizziness, blurred vision, headache, weakness, difficulty concentrating, slurred speech, and seizures in severe cases.
-
Neuroadrenergic Symptoms: These are triggered by the body's attempt to counteract low blood sugar. They can include sweating, palpitations, tremors, anxiety, and nervousness.
The severity of symptoms is often related to the rate and extent of blood glucose decline. Rapid drops are usually associated with more severe symptoms.
Management and Prevention of Hypoglycemia
The management of symptomatic hypoglycemia depends on the underlying cause. For patients with diabetes, careful monitoring of blood glucose levels, proper insulin dosing, regular meals, and awareness of potential triggers are essential. If hypoglycemia is caused by medication, an adjustment in dosage or a change of medication may be necessary under the guidance of a healthcare professional. Treating underlying medical conditions such as liver disease or endocrine disorders is crucial in managing hypoglycemia. In the case of insulinoma, surgical removal of the tumor is often the treatment of choice.
Prevention strategies involve educating patients about risk factors, promoting healthy lifestyle choices (including regular meals and balanced nutrition), and emphasizing the importance of regular blood glucose monitoring. Patients should be instructed on how to recognize and treat hypoglycemia promptly. Having readily available sources of fast-acting carbohydrates (like glucose tablets or juice) is crucial for managing episodes of low blood sugar.
Conclusion
Symptomatic hypoglycemia is a complex condition with multiple contributing factors. Understanding the patient profiles most at risk—those with diabetes, those taking certain medications, those with impaired glucose counter-regulation, and those with underlying medical conditions—is paramount for effective prevention and management. Early recognition of symptoms and prompt treatment are essential to mitigate the potential risks and complications associated with low blood sugar. Regular monitoring, adherence to treatment plans, and open communication with healthcare professionals are crucial for individuals at high risk of experiencing symptomatic hypoglycemia. Remember, this information is for educational purposes only and should not be considered medical advice. Always consult with a healthcare professional for diagnosis and treatment of any medical condition.
Latest Posts
Latest Posts
-
Which Condition Is A Contagious Inflammation Of The Eardrum
Mar 15, 2025
-
The Discharge Category Which Indicates Satisfactory Service
Mar 15, 2025
-
How Did Elevated Trains And Subways Improve Urban Transportation
Mar 15, 2025
-
Siphoning Of Wetlands In Iraq Has Led To
Mar 15, 2025
-
Patients With Perfusing Rhythms Should Receive Ventilations Once Every
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about Symptomatic Hypoglycemia Will Most Likely Develop If A Patient . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
