T Cells Achieve Self-tolerance In The __________.
Breaking News Today
Mar 26, 2025 · 6 min read
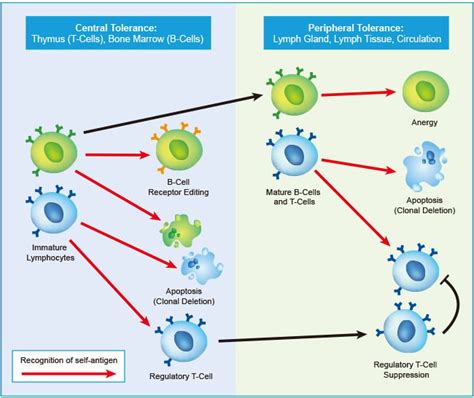
Table of Contents
T Cells Achieve Self-Tolerance in the Thymus: A Deep Dive into Central Tolerance
The immune system, a marvel of biological engineering, possesses the remarkable ability to distinguish between "self" and "non-self." This crucial distinction prevents the immune system from attacking the body's own tissues, a condition known as autoimmunity. Central to this self/non-self discrimination is the process of central tolerance, where self-reactive lymphocytes, primarily T cells, are eliminated or inactivated during their development. This critical process primarily occurs in the thymus. This article will delve deep into the mechanisms by which T cells achieve self-tolerance in the thymus, exploring the intricate processes of negative and positive selection, the roles of various thymic cells and molecules, and the implications of thymic tolerance failure in autoimmune diseases.
The Thymus: The School for T Cells
The thymus, a bi-lobed organ located in the mediastinum, is the primary site of T cell development and maturation. It's not just a passive location; the thymus actively shapes the T cell repertoire, ensuring that only self-tolerant T cells are released into the periphery to patrol the body. The thymus is comprised of distinct regions: the cortex and the medulla. Each region plays a crucial role in the different stages of T cell development and selection.
Thymic Microenvironment: A Symphony of Cellular Interactions
The thymus isn't just a collection of cells; it's a highly organized microenvironment teeming with diverse cell types that orchestrate T cell development and selection. These include:
-
Thymic epithelial cells (TECs): These are the keystone cells of the thymus, responsible for presenting self-antigens to developing T cells. They exist in two major subtypes: cortical thymic epithelial cells (cTECs) and medullary thymic epithelial cells (mTECs). cTECs are crucial for positive selection, while mTECs play a dominant role in negative selection.
-
Dendritic cells (DCs): These antigen-presenting cells capture and present self-antigens to developing T cells, contributing to both positive and negative selection.
-
Macrophages: These phagocytic cells remove apoptotic cells resulting from negative selection, maintaining thymic homeostasis.
This intricate network of cellular interactions ensures the efficient and precise selection of T cells that can both recognize foreign antigens and tolerate self-antigens.
Positive Selection: Ensuring Functionality
Before a T cell can even be considered for self-tolerance testing, it must first pass the test of functionality. This is achieved through positive selection, a process that occurs primarily in the thymic cortex. Here, developing T cells, known as thymocytes, interact with cTECs expressing major histocompatibility complex (MHC) molecules.
The MHC Restriction Test
T cell receptors (TCRs) on thymocytes must have a certain level of affinity for self-MHC molecules. This ensures that mature T cells can effectively interact with antigen-presenting cells (APCs) in the periphery, which also express MHC molecules. Thymocytes with TCRs that fail to bind to self-MHC molecules with sufficient avidity receive insufficient survival signals and undergo apoptosis. This process ensures that only T cells capable of recognizing antigens presented by self-MHC molecules survive.
Negative Selection: Eliminating Self-Reactivity
The crucial process of negative selection ensures that self-reactive T cells are eliminated, preventing autoimmunity. This occurs mainly in the thymic medulla, where thymocytes encounter a broader range of self-antigens presented by mTECs and DCs.
The Self-Tolerance Check
Thymocytes that strongly bind to self-antigens presented on MHC molecules receive signals that trigger apoptosis. This process eliminates T cells that have the potential to react against the body's own tissues. The strength of TCR binding to self-antigens is critical; weak binding leads to survival and potential peripheral tolerance, while strong binding triggers apoptosis.
Aided by AIRE: Autoimmune Regulator
The expression of a remarkable protein, AIRE (autoimmune regulator), is essential for the broad self-antigen repertoire presented in the thymic medulla. AIRE drives the ectopic expression of numerous tissue-specific genes in mTECs, allowing the presentation of a wide array of self-antigens. This ensures that T cells with high affinity for self-antigens from various tissues are effectively eliminated during negative selection. Defects in AIRE lead to autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED), a severe autoimmune disease highlighting the crucial role of AIRE in self-tolerance.
Regulatory T Cells (Tregs): Active Self-Tolerance
Beyond negative selection, another layer of self-tolerance is achieved through the generation of regulatory T cells (Tregs). Tregs are a specialized subset of T cells that actively suppress the activity of other self-reactive T cells that might have escaped negative selection. They are crucial for maintaining immune homeostasis and preventing autoimmunity. Their development in the thymus involves interactions with specific self-antigens and the expression of the transcription factor Foxp3. These thymic Tregs, also known as natural Tregs (nTregs), are critical for preventing autoimmunity.
Peripheral Tolerance: A Backup System
While central tolerance in the thymus eliminates the vast majority of self-reactive T cells, it isn't foolproof. Some self-reactive T cells may escape negative selection and enter the periphery. This is where peripheral tolerance mechanisms come into play. These mechanisms operate outside the thymus and help to suppress the activity of self-reactive T cells that manage to escape central tolerance. These mechanisms include:
-
Anergy: The inability of T cells to respond to antigen due to insufficient co-stimulation.
-
Deletion: Apoptosis of self-reactive T cells in the periphery.
-
Suppression by Tregs: The active suppression of self-reactive T cells by peripheral Tregs (induced Tregs or iTregs).
Failure of Thymic Tolerance: The Seeds of Autoimmunity
When the mechanisms of central and peripheral tolerance fail, the result can be devastating. Self-reactive T cells escape control and attack the body's own tissues, leading to autoimmune diseases. These diseases affect millions worldwide and can manifest in diverse ways, from organ-specific autoimmune diseases like type 1 diabetes and multiple sclerosis to systemic autoimmune diseases like lupus and rheumatoid arthritis. The precise reasons for thymic tolerance failure are complex and often involve a combination of genetic predisposition and environmental triggers.
Genetic Factors: Predisposition to Autoimmunity
Genetic variations can influence the efficiency of thymic selection and the development of Tregs. These variations can affect the expression of MHC molecules, TCRs, or key regulatory proteins, potentially leading to an increased risk of self-reactive T cells escaping central tolerance.
Environmental Factors: Triggering Autoimmunity
Environmental factors like infections, exposure to toxins, or stress can also contribute to thymic tolerance failure. These factors may alter the thymic microenvironment, influence the presentation of self-antigens, or trigger the activation of self-reactive T cells that have escaped central tolerance.
Conclusion: A Complex, Vital Process
The achievement of self-tolerance in the thymus is a remarkably complex and precise process, essential for maintaining immune homeostasis and preventing autoimmunity. The intricate interplay of thymic epithelial cells, dendritic cells, macrophages, and the mechanisms of positive and negative selection, aided by AIRE and Tregs, ensures that only self-tolerant T cells are released into the periphery. Understanding the mechanisms of thymic tolerance is crucial for developing effective strategies to treat and prevent autoimmune diseases. Ongoing research continues to unravel the intricate details of this process, offering hope for future advancements in the treatment and prevention of these devastating conditions. Further exploration into the interplay of genetic and environmental factors is needed to gain a more comprehensive understanding of the causes of thymic tolerance failure and the development of autoimmune diseases. This knowledge will ultimately lead to more effective therapies and preventative measures for these challenging conditions.
Latest Posts
Latest Posts
-
El Nacimiento Es El Fin De La Vida
Mar 29, 2025
-
A 26 Year Old Female Presents With Heavy Vaginal Bleeding
Mar 29, 2025
-
Suspected Ethics Violations Should Be Reported To
Mar 29, 2025
-
Tension Has A Dynamic Aesthetic Quality Which
Mar 29, 2025
-
Why Did The Supreme Court Rule Against Archbishop Flores
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about T Cells Achieve Self-tolerance In The __________. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
