The Most Reliable Indicator Of An Underlying Fracture Is
Breaking News Today
Mar 15, 2025 · 6 min read
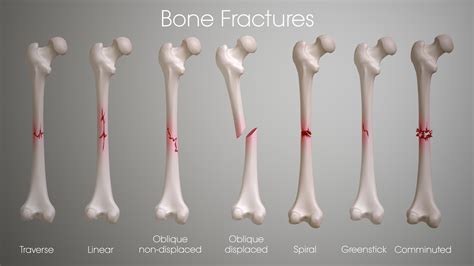
Table of Contents
The Most Reliable Indicator of an Underlying Fracture is…
Determining the presence of an underlying fracture can be a complex diagnostic challenge, especially in cases where the injury isn't immediately obvious. While various symptoms and imaging techniques contribute to the diagnosis, the most reliable indicator remains a combination of clinical examination findings and imaging evidence, specifically high-resolution imaging modalities such as X-rays, CT scans, and MRI scans. This article will delve into the specifics of identifying fractures, highlighting the crucial role of a comprehensive approach.
Understanding Fractures: A Primer
Before exploring the most reliable indicators, let's establish a foundational understanding of fractures. A fracture is a break in the continuity of a bone. These breaks can range in severity from a simple hairline crack (stress fracture) to a completely shattered bone (comminuted fracture). The location, type, and severity of the fracture significantly influence the diagnostic process and subsequent treatment. Several factors contribute to fracture occurrence, including:
- Trauma: High-impact accidents, falls, sports injuries, and direct blows are common causes.
- Osteoporosis: Weakening of the bones due to age or disease increases fracture susceptibility.
- Pathological fractures: Underlying bone diseases (e.g., bone cancer) can weaken the bone, leading to fractures even with minimal trauma.
- Stress fractures: Repetitive stress on a bone, often seen in athletes, can cause tiny cracks.
Clinical Examination: The First Step
The initial assessment of a suspected fracture starts with a thorough clinical examination conducted by a healthcare professional. This examination is crucial because it provides vital clues even before any imaging is performed. Key components of this examination include:
1. Patient History: Unveiling the Narrative
A comprehensive history taking is paramount. The doctor will inquire about:
- Mechanism of injury: How did the injury occur? Understanding the forces involved helps predict the potential location and type of fracture.
- Pain characteristics: Location, intensity, onset, and nature of the pain (sharp, dull, aching) offer valuable insights.
- Swelling and bruising: These are common signs of inflammation and tissue damage associated with fractures.
- Functional limitations: Is the patient able to bear weight, move the limb, or perform normal activities? Loss of function is a strong indicator.
- Past medical history: Conditions like osteoporosis or bone cancer can increase the likelihood of a fracture.
2. Physical Examination: Visual and Palpatory Assessment
The physical examination involves:
- Visual inspection: Assessing for deformities, swelling, bruising, and abnormal limb positioning.
- Palpation: Carefully feeling the bone for tenderness, crepitus (a grating sound or sensation indicating bone fragments rubbing together), and instability.
- Range of motion testing: Assessing the joint's ability to move through its normal range, noting any limitations or pain during movement.
- Neurovascular assessment: Checking for signs of nerve or blood vessel damage in the affected area.
Imaging Techniques: Visualizing the Fracture
While the clinical examination is crucial, imaging techniques provide definitive confirmation of the fracture and detailed information about its location, type, and extent.
1. X-rays: The Workhorse of Fracture Diagnosis
X-rays remain the initial and most frequently used imaging modality for fracture detection. They utilize ionizing radiation to produce images of bone density. X-rays are excellent at identifying:
- Displaced fractures: Where the bone fragments are out of alignment.
- Simple fractures: Clean breaks in the bone.
- Comminuted fractures: Fractures with multiple bone fragments.
- Avulsion fractures: Fractures where a piece of bone is pulled away from the main bone.
However, X-rays have limitations:
- Stress fractures: May not be visible on initial X-rays, requiring follow-up imaging.
- Soft tissue injuries: X-rays primarily visualize bone and don't show soft tissue damage (ligaments, tendons, muscles).
2. CT Scans: High-Resolution 3D Imaging
Computed tomography (CT) scans provide detailed cross-sectional images of the bone, offering superior visualization compared to X-rays. CT scans are particularly useful in:
- Complex fractures: Providing precise detail of comminuted fractures and bone fragments.
- Pelvic fractures: Assessing the intricate structure of the pelvis.
- Vertebral fractures: Detecting subtle fractures in the spine.
3. MRI Scans: Assessing Soft Tissue Injuries
Magnetic resonance imaging (MRI) scans use magnetic fields and radio waves to produce detailed images of both bone and soft tissues. MRI scans are invaluable in:
- Stress fractures: Detecting subtle bone marrow edema (swelling) indicative of stress fractures.
- Ligament and tendon injuries: Assessing associated soft tissue damage, which is often present with fractures.
- Osteonecrosis: Detecting bone death due to reduced blood supply.
The Most Reliable Indicator: A Synergistic Approach
The most reliable indicator of an underlying fracture isn't a single test or finding, but rather the integration of clinical findings and imaging evidence. A healthcare professional will consider the following in reaching a diagnosis:
- High clinical suspicion: A detailed history consistent with a fracture and physical examination findings like tenderness, deformity, or crepitus increase the likelihood.
- Positive imaging findings: X-rays, CT scans, or MRI scans definitively confirming the presence of a fracture.
- Correlation between clinical findings and imaging: The imaging findings should correlate with the patient's symptoms and physical examination results. For example, a patient with pain over a specific bone and a fracture visible on the X-ray in that precise location supports the diagnosis.
- Exclusion of alternative diagnoses: The healthcare professional needs to rule out other potential causes of the patient's symptoms, such as muscle strains, sprains, or other injuries.
Specific Examples and Case Studies
Let's consider hypothetical scenarios to illustrate the interplay between clinical examination and imaging:
Case 1: Ankle Injury after a Fall
A patient presents with severe ankle pain, swelling, and inability to bear weight after a fall. The physical examination reveals tenderness over the lateral malleolus (outer ankle bone), and there's palpable instability. The X-ray shows a fracture of the fibula. The combination of clinical findings (pain, swelling, instability) and the positive X-ray finding strongly suggests an ankle fracture.
Case 2: Athlete with Gradual Onset of Leg Pain
An athlete complains of persistent, dull pain in the lower leg after several weeks of intense training. The physical examination reveals localized tenderness but no obvious deformity. Initial X-rays are negative. However, an MRI scan reveals a stress fracture of the tibia. In this case, the initial X-ray was inconclusive, but the MRI provided definitive evidence consistent with the patient’s history and physical findings.
Case 3: Elderly Patient with Hip Pain after a Minor Fall
An elderly patient with osteoporosis falls and experiences hip pain. The physical examination reveals tenderness over the greater trochanter and limited range of motion. The X-ray shows a fracture of the femoral neck. In this case, the combination of the patient's osteoporosis (predisposing factor), fall (mechanism of injury), and the positive X-ray result confirmed the hip fracture.
Conclusion: Integrating Evidence for Accurate Diagnosis
In conclusion, the most reliable indicator of an underlying fracture is not a single element but rather the synergistic integration of a comprehensive clinical examination and appropriate imaging studies. A healthcare professional meticulously assesses the patient's history, conducts a thorough physical examination, and utilizes advanced imaging techniques to confirm the diagnosis and accurately characterize the fracture. This integrated approach minimizes the risk of misdiagnosis, ensuring appropriate treatment and patient care. The key to accurate diagnosis lies in the skillful interpretation of the collected evidence, leading to optimal management of fractures and improved patient outcomes. Remember, self-diagnosis is never advisable, and timely consultation with a healthcare professional is crucial for any suspected fracture.
Latest Posts
Latest Posts
-
How Did Elevated Trains And Subways Improve Urban Transportation
Mar 15, 2025
-
Siphoning Of Wetlands In Iraq Has Led To
Mar 15, 2025
-
Patients With Perfusing Rhythms Should Receive Ventilations Once Every
Mar 15, 2025
-
In A State Supervised County Administered State
Mar 15, 2025
-
How Quickly Should You Move During Resistance Training
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about The Most Reliable Indicator Of An Underlying Fracture Is . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
