The Oldest And Most Frequently Prescribed Drugs For Angina Are
Breaking News Today
Mar 27, 2025 · 6 min read
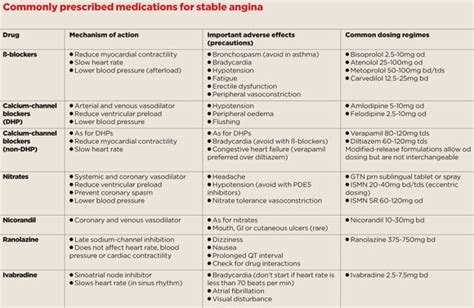
Table of Contents
The Oldest and Most Frequently Prescribed Drugs for Angina: A Comprehensive Review
Angina pectoris, commonly known as angina, is a symptom of coronary artery disease (CAD). It manifests as chest pain or discomfort due to reduced blood flow to the heart muscle. While modern medicine offers a range of treatments, understanding the oldest and most frequently prescribed drugs for angina provides valuable insight into the evolution of cardiovascular care and the cornerstone therapies still relied upon today. This article will delve into these medications, exploring their mechanisms of action, efficacy, side effects, and current place in clinical practice.
Nitrates: The Pioneers in Angina Treatment
Nitrates have a long and storied history in angina management, representing some of the oldest drugs used to treat the condition. Their use dates back centuries, with observations of the vasodilatory properties of nitrates in various plant extracts. Today, nitrates remain a mainstay of angina therapy, particularly for managing acute attacks.
Mechanisms of Action:
Nitrates exert their therapeutic effects primarily through the release of nitric oxide (NO). NO is a potent vasodilator, meaning it relaxes and widens blood vessels. This vasodilation has several beneficial effects in angina:
- Reduced Preload: By dilating veins, nitrates decrease the amount of blood returning to the heart (preload). This reduces the workload on the heart, lessening the oxygen demand.
- Reduced Afterload: Dilating arteries, particularly arterioles, lowers the resistance the heart must overcome to pump blood (afterload). This also reduces the heart's oxygen demand.
- Improved Coronary Blood Flow: While the primary effect isn't direct coronary dilation, the overall reduction in cardiac workload and improved systemic circulation can contribute to improved blood flow to the ischemic myocardium.
Types of Nitrates:
Several nitrate formulations exist, each tailored to different treatment needs:
- Sublingual Nitroglycerin: This fast-acting form is administered under the tongue for rapid relief of acute angina attacks. It provides quick relief due to its rapid absorption through the oral mucosa.
- Oral Nitroglycerin: Sustained-release oral formulations are used for prophylaxis, preventing angina attacks. These provide a more prolonged effect than sublingual nitroglycerin.
- Transdermal Nitroglycerin Patches: These patches deliver a continuous supply of nitroglycerin through the skin, offering around-the-clock prophylaxis. They are particularly useful for preventing angina during periods of increased activity or stress.
- Intravenous Nitroglycerin: Used in hospital settings for the management of severe angina, particularly during acute coronary syndromes. Intravenous administration allows for precise titration of the dose.
Side Effects:
While generally safe and effective, nitrates can cause several side effects, including:
- Headache: This is a common side effect, often due to vasodilation in cerebral blood vessels. It usually diminishes with continued use.
- Hypotension: Nitrates can cause a significant drop in blood pressure, particularly in patients with already low blood pressure or those taking other vasodilators.
- Reflex Tachycardia: The decrease in blood pressure can trigger an increase in heart rate (tachycardia) as the body attempts to compensate.
- Tolerance: With prolonged use, tolerance to nitrates can develop, requiring dose adjustments or alternative therapies.
Beta-Blockers: Managing Heart Rate and Contractility
Beta-blockers represent another class of drugs with a long history in angina management. They are effective in reducing the heart's workload and oxygen demand, thereby alleviating angina symptoms.
Mechanisms of Action:
Beta-blockers work by blocking the effects of catecholamines (epinephrine and norepinephrine) on beta-adrenergic receptors in the heart. This action leads to several beneficial effects:
- Reduced Heart Rate: Beta-blockers slow the heart rate, decreasing the oxygen demand of the heart.
- Reduced Contractility: They decrease the force of myocardial contractions, further lowering oxygen demand.
- Reduced Blood Pressure: In some cases, beta-blockers can also lower blood pressure, contributing to reduced cardiac workload.
Types of Beta-Blockers:
Various beta-blockers are available, each with its own pharmacological profile and selectivity for beta-1 (cardiac) and beta-2 (bronchial) receptors:
- Non-selective beta-blockers: Affect both beta-1 and beta-2 receptors. These are generally avoided in patients with asthma or chronic obstructive pulmonary disease (COPD) due to the risk of bronchospasm.
- Selective beta-1 blockers: Primarily affect beta-1 receptors, minimizing the risk of bronchospasm. These are generally preferred in patients with respiratory conditions.
Side Effects:
Common side effects of beta-blockers include:
- Bradycardia: Slow heart rate.
- Hypotension: Low blood pressure.
- Fatigue: Tiredness and weakness.
- Bronchospasm: In patients with asthma or COPD, particularly with non-selective beta-blockers.
- Depression: While not common, some patients may experience depression.
Calcium Channel Blockers: Dilating Arteries and Reducing Contractility
Calcium channel blockers (CCBs) are another important class of drugs used in angina treatment. They work by inhibiting the influx of calcium ions into vascular smooth muscle cells and cardiac myocytes.
Mechanisms of Action:
CCBs exert their effects through several mechanisms:
- Vasodilation: By reducing calcium influx into vascular smooth muscle cells, CCBs cause vasodilation, reducing both preload and afterload.
- Reduced Contractility: In the heart, CCBs can reduce the force of myocardial contractions, lowering oxygen demand.
- Improved Coronary Blood Flow: Some CCBs, particularly dihydropyridines, have a more pronounced effect on peripheral vasodilation, indirectly improving coronary blood flow.
Types of Calcium Channel Blockers:
Two main types of CCBs are used in angina:
- Dihydropyridines (e.g., amlodipine, nifedipine): These primarily affect vascular smooth muscle, causing vasodilation.
- Non-dihydropyridines (e.g., verapamil, diltiazem): These have effects on both vascular smooth muscle and cardiac myocytes, causing vasodilation and reducing contractility.
Side Effects:
Side effects of CCBs can include:
- Headache: Common, especially with dihydropyridines.
- Edema: Fluid retention, particularly in the ankles and feet.
- Hypotension: Low blood pressure.
- Bradycardia: Slow heart rate, more common with non-dihydropyridines.
- Constipation: More common with non-dihydropyridines.
Ranolazine: A Newer Addition to Angina Management
Ranolazine is a relatively newer addition to the therapeutic armamentarium for angina. It differs mechanistically from the older agents, offering a unique approach to managing angina.
Mechanisms of Action:
Ranolazine's primary mechanism of action involves inhibiting the late sodium current in cardiac myocytes. This reduces the amount of calcium entering the cells during depolarization. The net effect is a reduction in myocardial oxygen demand. Importantly, it doesn't significantly affect heart rate or blood pressure.
Side Effects:
Common side effects of ranolazine include:
- Nausea: A relatively common side effect.
- Constipation: Can occur in some patients.
- Dizziness: May be experienced by some individuals.
- QT interval prolongation: Ranolazine can prolong the QT interval on electrocardiograms (ECGs), requiring caution in patients with pre-existing QT prolongation.
Choosing the Right Angina Medication: A Multifaceted Approach
The selection of the most appropriate angina medication depends on several factors, including:
- Severity of Angina: For acute attacks, sublingual nitroglycerin is the first-line treatment. For chronic stable angina, prophylactic medications like beta-blockers, CCBs, or ranolazine are used.
- Patient-Specific Factors: Comorbidities like asthma, COPD, or heart failure influence medication choice. Renal or hepatic impairment also necessitates careful consideration of drug selection and dosage.
- Individual Response: The effectiveness and tolerability of medications vary between individuals. Titration of dosage and monitoring of side effects are crucial.
- Combined Therapy: Often, a combination of drugs is used to optimize angina control. For instance, a beta-blocker and a CCB might be used together.
Conclusion: A Legacy of Innovation in Angina Treatment
The oldest and most frequently prescribed drugs for angina—nitrates, beta-blockers, and calcium channel blockers—represent a legacy of pharmaceutical innovation in cardiovascular care. Their mechanisms of action, efficacy, and side effect profiles have been extensively studied, shaping current clinical practice. While newer agents like ranolazine offer additional therapeutic options, the older drugs remain cornerstones of angina management. Selecting the appropriate medication requires a careful consideration of the patient's specific clinical presentation, comorbidities, and individual responses to therapy. Ongoing research continues to refine our understanding of angina pathophysiology and treatment, promising further advancements in managing this prevalent cardiovascular condition.
Latest Posts
Latest Posts
-
The Government Engages In An Industrial Policy
Mar 30, 2025
-
Discuss The Interdependence Of The Components Of Wellness
Mar 30, 2025
-
Which Statement Is Not True About Receipts
Mar 30, 2025
-
True Or False Osmosis Is A Type Of Diffusion
Mar 30, 2025
-
Most Surface Ocean Waves Are Caused By
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about The Oldest And Most Frequently Prescribed Drugs For Angina Are . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
