The Patient Is Showing Persistent Pulseless Ventricular Tachycardia
Breaking News Today
Mar 29, 2025 · 6 min read
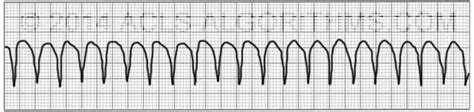
Table of Contents
The Patient is Showing Persistent Pulseless Ventricular Tachycardia: A Comprehensive Guide for Healthcare Professionals
Pulseless ventricular tachycardia (pVT) is a life-threatening cardiac arrhythmia characterized by a rapid, chaotic ventricular rhythm without palpable pulses. Its persistence signifies a critical situation requiring immediate intervention, as it represents a form of cardiac arrest. This comprehensive guide delves into the understanding, diagnosis, management, and prognosis of persistent pVT, focusing on crucial aspects for healthcare professionals.
Understanding Pulseless Ventricular Tachycardia (pVT)
What is Ventricular Tachycardia (VT)? Ventricular tachycardia is a heart rhythm disorder where the ventricles beat rapidly and irregularly. The heart rate can exceed 100 beats per minute, sometimes reaching much higher rates. While some forms of VT can be relatively benign, pulseless VT represents a severe form that compromises cardiac output.
The Significance of "Pulseless": The key differentiator between VT and pVT is the absence of a palpable pulse. This means the heart's contractions are ineffective at pumping blood to the body, leading to a state of cardiac arrest. This lack of effective circulation causes rapid deterioration in organ function and ultimately, death if not addressed immediately.
Mechanism of pVT: pVT arises from abnormal electrical activity within the ventricles. This can be triggered by various factors, including:
- Myocardial Ischemia: Reduced blood flow to the heart muscle, often due to coronary artery disease, is a leading cause. The ischemic myocardium becomes more susceptible to generating abnormal electrical impulses.
- Myocardial Infarction: A heart attack, where a portion of the heart muscle dies due to lack of blood flow, is a major risk factor for pVT. The damaged tissue can disrupt the heart's electrical conduction system.
- Cardiomyopathies: Diseases affecting the heart muscle structure and function, such as dilated cardiomyopathy and hypertrophic cardiomyopathy, can increase the risk of pVT.
- Electrolyte Imbalances: Disturbances in electrolytes like potassium, magnesium, and calcium can disrupt the heart's electrical activity, potentially leading to pVT.
- Drug Toxicity: Certain medications, especially those affecting the heart's rhythm, can trigger pVT.
- Structural Heart Disease: Conditions like congenital heart defects or valvular heart disease can create an environment conducive to arrhythmias like pVT.
- Genetic Predisposition: Certain genetic mutations can increase the risk of developing VT and pVT.
Recognizing and Diagnosing Persistent pVT
Clinical Presentation: The hallmark of pVT is the abrupt loss of consciousness, absence of a pulse, and lack of breathing or gasping respirations. The patient will be unresponsive and show no signs of circulation. This is a critical situation that requires immediate action.
Electrocardiogram (ECG): The ECG is the cornerstone of diagnosing pVT. It reveals a rapid, wide-complex tachycardia with no discernible P waves (representing atrial activity) and absence of organized QRS complexes. The morphology of the QRS complexes can provide clues about the underlying cause. The persistence of this rhythm emphasizes the severity.
Differential Diagnosis: It's crucial to differentiate pVT from other life-threatening conditions that might present with similar symptoms:
- Pulseless Electrical Activity (PEA): PEA shows organized electrical activity on the ECG but lacks a palpable pulse. The underlying cause differs significantly from pVT.
- Asystole: This is the complete absence of electrical activity in the heart, a more severe condition.
- Other Shock States: Hypovolemic shock, septic shock, and cardiogenic shock can present with a weak or absent pulse, requiring careful differentiation.
Immediate Management of Persistent pVT
The immediate management of persistent pVT is a critical time-sensitive intervention focusing on restoring effective circulation. The primary treatment is cardiopulmonary resuscitation (CPR) followed by defibrillation.
1. Cardiopulmonary Resuscitation (CPR): High-quality CPR should be initiated immediately upon recognition of pVT. This involves chest compressions and rescue breathing, aiming for adequate chest compressions at a rate of at least 100-120 compressions per minute with minimal interruptions.
2. Defibrillation: Immediate defibrillation is the most effective treatment for pVT. A high-energy shock (typically 200 joules or higher) should be delivered, followed by immediate resumption of CPR. Repeated defibrillation may be necessary.
3. Advanced Cardiovascular Life Support (ACLS) Medications: After defibrillation and CPR, ACLS medications may be administered, including:
- Amiodarone: This antiarrhythmic medication is often the first choice to help restore a normal heart rhythm.
- Lidocaine: Another antiarrhythmic drug that can be effective in treating VT.
- Magnesium Sulfate: This may be beneficial in cases where electrolyte imbalances are suspected.
- Epinephrine: Used to improve cardiac contractility and increase blood pressure during CPR.
Post-Resuscitation Management of Persistent pVT
Once a pulse is restored, the focus shifts to stabilization and identification of the underlying cause. This involves:
- Continuous ECG Monitoring: To detect any recurrence of pVT or other arrhythmias.
- Hemodynamic Monitoring: To assess blood pressure, heart rate, and oxygen saturation.
- Laboratory Investigations: Blood tests to evaluate electrolyte levels, cardiac enzymes (to assess for myocardial damage), and other relevant markers.
- Echocardiography: An ultrasound of the heart to assess the heart's structure and function, identifying potential causes like structural heart disease.
- Coronary Angiography: If coronary artery disease is suspected, coronary angiography may be performed to visualize the coronary arteries and assess for blockages.
Underlying Cause Management
Addressing the underlying cause of pVT is crucial for long-term management. This may involve various interventions depending on the specific etiology:
- Percutaneous Coronary Intervention (PCI): If coronary artery disease is identified, PCI may be necessary to open blocked arteries.
- Coronary Artery Bypass Graft (CABG): In cases of significant coronary artery disease, CABG surgery may be required.
- Medication Management: Ongoing medications may be prescribed to manage underlying conditions, including antiarrhythmic drugs to prevent recurrence of VT.
- Implantable Cardioverter-Defibrillator (ICD): An ICD may be implanted to deliver shocks automatically if VT or ventricular fibrillation recurs.
Prognosis and Long-Term Outlook
The prognosis of patients who experience persistent pVT depends heavily on the underlying cause, the effectiveness of the resuscitation efforts, and the presence of any existing comorbidities. Early intervention and effective resuscitation dramatically improve the chances of survival. However, the risk of recurrence and long-term complications remains significant. Patients often require ongoing monitoring and management, including regular check-ups, medication, and possibly an ICD. Cardiac rehabilitation plays a vital role in improving functional capacity and overall quality of life.
Conclusion
Persistent pulseless ventricular tachycardia is a critical cardiac emergency requiring immediate and coordinated action. Prompt recognition, initiation of CPR, and immediate defibrillation are crucial for improving survival rates. Understanding the underlying causes and implementing appropriate management strategies significantly influence the patient's long-term prognosis. Continuous ECG monitoring, post-resuscitation care, and ongoing management of the underlying conditions are all essential components in improving the long-term outcome for patients experiencing this life-threatening arrhythmia. Healthcare professionals should be well-versed in the diagnostic criteria, treatment protocols, and post-resuscitation management to effectively manage this critical situation and optimize patient outcomes. The emphasis on preventative measures and early recognition cannot be understated in mitigating the risks associated with this potentially fatal cardiac event.
Latest Posts
Latest Posts
-
A Specific Problem That Atherosclerosis Can Cause Is Quizlet
Mar 31, 2025
-
Acute Kidney Failure Can Be Reversed With Quizlet
Mar 31, 2025
-
Adhd Is A Disorder That Is Quizlet
Mar 31, 2025
-
Which Statement Concerning Rare Threatened Or Endangered Species Is True
Mar 31, 2025
-
Defining Research With Human Subjects Citi Quizlet
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about The Patient Is Showing Persistent Pulseless Ventricular Tachycardia . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
