Tina Jones Respiratory Shadow Health Objective Data
Breaking News Today
Mar 26, 2025 · 7 min read
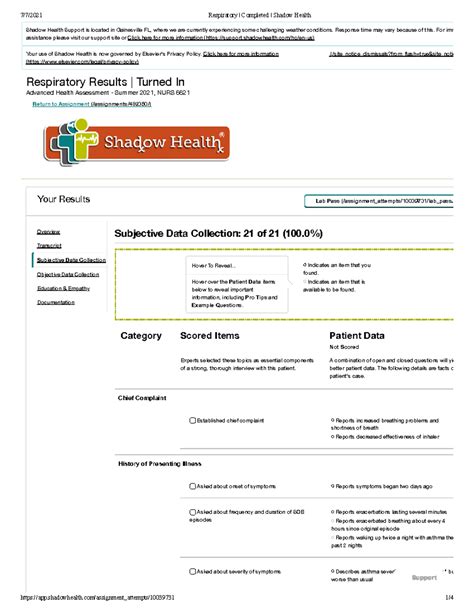
Table of Contents
Tina Jones Respiratory Shadow Health: A Comprehensive Objective Data Analysis
Shadow Health's Tina Jones case study provides a rich, simulated experience for healthcare students learning to assess and diagnose respiratory conditions. This detailed analysis focuses on the objective data presented in Tina Jones' respiratory assessment, exploring the significance of each finding and how they contribute to a comprehensive understanding of her condition. We will delve into the physical examination findings, laboratory results (where applicable), and imaging studies, connecting these elements to potential diagnoses and appropriate nursing interventions.
I. Physical Examination Findings: The Cornerstones of Objective Data
The physical examination forms the bedrock of objective data collection in any respiratory assessment. Tina Jones' case study presents a range of observable and measurable findings crucial to forming a differential diagnosis. Let's break down the key components:
A. Vital Signs: The Initial Clues
Vital signs, the simplest yet often most revealing indicators, provide initial insights into Tina's respiratory status. We need to consider:
- Heart Rate (HR): An elevated HR might indicate the body's compensatory response to hypoxia or respiratory distress. A normal HR, however, doesn't rule out respiratory issues. The context of other findings is essential.
- Respiratory Rate (RR): Tachypnea (increased RR) is a classic sign of respiratory compromise. The depth and rhythm of breathing (e.g., shallow breathing, use of accessory muscles) are equally important.
- Blood Pressure (BP): Hypertension or hypotension could signal underlying conditions exacerbating respiratory problems or indicate the severity of the illness.
- Temperature: Fever suggests an infectious process, a common cause of respiratory issues. Hypothermia, while less common, can also accompany severe respiratory illnesses.
- Oxygen Saturation (SpO2): Hypoxemia (low blood oxygen levels), indicated by a low SpO2, is a critical finding requiring immediate attention. The severity of hypoxemia dictates the urgency of intervention.
B. Respiratory Assessment: Listening, Looking, and Feeling
A thorough respiratory assessment involves several techniques:
- Inspection: Observe the patient's respiratory effort, noting any use of accessory muscles (e.g., sternocleidomastoids, intercostals), nasal flaring, or paradoxical breathing. Assess for any visible distress, such as cyanosis (bluish discoloration of the skin and mucous membranes).
- Palpation: Palpate the chest wall to assess for tactile fremitus (vibrations felt during speech), tenderness, or any abnormalities in chest expansion. Unequal expansion suggests underlying lung pathology.
- Percussion: Percuss the chest to determine the density of the underlying lung tissue. Dullness might indicate consolidation (fluid or solid mass in the lungs), while hyperresonance suggests air trapping (e.g., in emphysema).
- Auscultation: Auscultate the lungs systematically, listening for normal breath sounds, adventitious sounds (e.g., crackles, wheezes, rhonchi, pleural rubs), and any diminished or absent breath sounds. The location, quality, and timing of these sounds are crucial in identifying the underlying pathology. For example, crackles might suggest pneumonia or pulmonary edema, wheezes suggest bronchospasm (asthma), and rhonchi suggest secretions in the airways.
C. Cardiovascular Assessment: Interconnected Systems
Respiratory and cardiovascular systems are intimately linked. Assessing the cardiovascular system can provide valuable insights into the patient's overall condition. Key aspects include:
- Heart sounds: Auscultate the heart for any murmurs, gallops, or other abnormal sounds that might indicate cardiac involvement in the patient's respiratory distress.
- Peripheral pulses: Assess peripheral pulses for rate, rhythm, and strength. Weak or absent pulses might indicate poor perfusion related to the respiratory compromise.
- Jugular venous distension (JVD): JVD can indicate increased right atrial pressure, potentially secondary to pulmonary hypertension or right-sided heart failure, both of which can affect respiratory function.
II. Laboratory Data: Objective Markers of Disease
Laboratory data, while not always included in a comprehensive physical exam, provides objective markers of inflammation, infection, and other physiological processes. Important lab tests related to Tina Jones’ respiratory condition might include:
- Complete Blood Count (CBC): Elevated white blood cell count (leukocytosis) might indicate infection. Anemia (low red blood cell count) could contribute to fatigue and reduced oxygen-carrying capacity.
- Arterial Blood Gas (ABG): ABG analysis directly measures blood oxygen and carbon dioxide levels, providing precise data on the severity of hypoxemia or hypercapnia (elevated carbon dioxide levels). It also assesses blood pH, indicating the presence of acidosis or alkalosis.
- Electrolytes: Electrolyte imbalances, particularly potassium and sodium, can impact respiratory muscle function and overall cardiac function.
- C-reactive protein (CRP): CRP is an inflammatory marker. Elevated levels suggest inflammation in the body, potentially related to an infection or other inflammatory process.
- Procalcitonin (PCT): PCT is a specific marker of bacterial infection. Elevated levels suggest a bacterial rather than a viral infection.
- Blood cultures: If infection is suspected, blood cultures are essential to identify the causative organism and guide appropriate antibiotic therapy.
- Sputum culture and sensitivity: If sputum is available, culture and sensitivity testing can identify the infecting organism and determine its susceptibility to various antibiotics.
III. Imaging Studies: Visualizing the Respiratory System
Imaging studies offer valuable visual information about the structures and function of the respiratory system. For Tina Jones, relevant imaging studies might include:
- Chest X-ray (CXR): A CXR provides a relatively quick and readily available image of the lungs, heart, and surrounding structures. It can reveal infiltrates (areas of consolidation), pleural effusions (fluid in the pleural space), pneumothorax (collapsed lung), atelectasis (collapsed lung segment), or other abnormalities.
- Computed Tomography (CT) Scan: A CT scan offers a more detailed view of the lungs than a CXR, allowing for better visualization of small lesions or abnormalities. It can be helpful in evaluating complex respiratory conditions.
- High-resolution CT (HRCT) scan: HRCT scans are especially useful for identifying interstitial lung diseases.
- Pulmonary function tests (PFTs): These tests assess lung volumes, capacities, and flows to evaluate the severity and type of lung disease. This data is important for assessing the severity of conditions such as asthma or COPD.
IV. Synthesizing the Objective Data: Towards a Differential Diagnosis
Combining the physical examination findings, laboratory results, and imaging data allows for the development of a differential diagnosis – a list of possible conditions that could explain Tina Jones’ symptoms. The specific findings in Tina's case would dictate which conditions are most likely. Possible differential diagnoses for respiratory problems could include:
- Pneumonia: Characterized by inflammation and infection of the lung parenchyma, pneumonia would likely manifest with fever, cough, sputum production, crackles on auscultation, and infiltrates on CXR. Elevated white blood cell count and positive sputum culture would further support the diagnosis.
- Acute bronchitis: Inflammation of the bronchi, acute bronchitis often presents with cough, sputum production, and wheezing. CXR typically appears normal.
- Asthma: Characterized by airway inflammation and bronchospasm, asthma presents with wheezing, shortness of breath, and cough. PFTs may show reduced airflow.
- Chronic obstructive pulmonary disease (COPD): An umbrella term for chronic bronchitis and emphysema, COPD is characterized by airflow limitation. Patients often have a chronic cough, sputum production, and dyspnea. PFTs would demonstrate obstructive airflow patterns.
- Pulmonary embolism (PE): A blood clot in the pulmonary arteries, PE can cause sudden shortness of breath, chest pain, and tachycardia. Diagnosis usually involves imaging studies (CT pulmonary angiography) and blood tests to assess for coagulation disorders.
- Pleurisy: Inflammation of the pleura (the lining of the lungs and chest cavity) causing sharp chest pain worsened by breathing. A pleural rub might be auscultated.
- Lung cancer: A serious condition that can present with cough, hemoptysis (coughing up blood), and weight loss. Imaging studies are crucial for diagnosis.
V. The Importance of Subjectivity: Bridging Objective and Subjective Data
While this analysis focuses on objective data, it's crucial to remember the importance of subjective data (symptoms reported by the patient) in forming a complete clinical picture. Tina Jones’ reported symptoms – such as cough, shortness of breath, chest pain, and fatigue – need to be integrated with the objective findings to arrive at an accurate diagnosis and plan of care. For example, the character and timing of her cough, the severity and triggers of her shortness of breath, and the location and quality of her chest pain are all essential pieces of the puzzle.
VI. Conclusion: A Holistic Approach to Respiratory Assessment
Assessing Tina Jones' respiratory status requires a comprehensive and holistic approach. Meticulous collection and interpretation of objective data – from vital signs and physical examination findings to laboratory results and imaging studies – are crucial steps in formulating a differential diagnosis and developing a plan of care. However, it is paramount to remember that objective data must always be interpreted in conjunction with the patient's subjective experience to ensure a thorough and accurate assessment. By integrating both objective and subjective information, healthcare providers can effectively diagnose and manage respiratory conditions, ensuring optimal patient outcomes. The Shadow Health simulation provides a valuable platform to practice these skills in a safe and controlled environment.
Latest Posts
Latest Posts
-
Which Industry Did The Interstate Commerce Act Primarily Affect
Mar 29, 2025
-
Ap Chem Unit 5 Progress Check Mcq
Mar 29, 2025
-
Which Of These Are True Of Tests For Online Courses
Mar 29, 2025
-
Drug Addiction Is A Clinical Diagnosis That Everfi
Mar 29, 2025
-
El Nacimiento Es El Fin De La Vida
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Respiratory Shadow Health Objective Data . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
