What Is The Dose For Emergency Volume Expander
Breaking News Today
Mar 16, 2025 · 5 min read
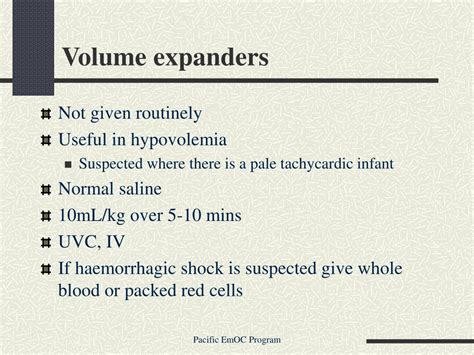
Table of Contents
What is the Dose for Emergency Volume Expanders?
Fluid resuscitation is a cornerstone of emergency medicine, crucial for stabilizing patients experiencing hypovolemic shock. The selection and dosage of volume expanders, however, are complex decisions requiring careful consideration of the patient's specific condition, the severity of fluid loss, and the type of expander used. There's no single "correct" dose; optimal fluid management is a dynamic process demanding continuous monitoring and adjustment. This article explores the intricacies of emergency volume expander dosage, emphasizing the importance of individualized treatment.
Understanding Hypovolemic Shock and Fluid Resuscitation
Hypovolemic shock arises from a significant reduction in circulating blood volume, leading to inadequate tissue perfusion. This can stem from various causes, including hemorrhage (trauma, internal bleeding), severe dehydration (vomiting, diarrhea), burns, and sepsis. Effective fluid resuscitation aims to restore circulating volume, improve tissue perfusion, and stabilize hemodynamic parameters (blood pressure, heart rate).
Types of Volume Expanders
Several types of intravenous fluids are used as volume expanders, each with its own characteristics, advantages, and limitations:
1. Crystalloids: These solutions contain water, electrolytes (sodium, chloride, potassium), and sometimes dextrose. They distribute throughout the entire extracellular fluid space (intravascular and interstitial). Examples include:
- Normal Saline (0.9% NaCl): A commonly used isotonic crystalloid, readily available and inexpensive.
- Lactated Ringer's (LR): An isotonic crystalloid containing lactate, which the liver metabolizes to bicarbonate, helping to buffer acidosis.
- Dextrose solutions: These provide energy but may contribute to hyperglycemia. They're often combined with other fluids.
2. Colloids: These solutions contain large molecules (proteins or synthetic polymers) that remain primarily within the intravascular space, offering a more sustained increase in plasma volume compared to crystalloids. Examples include:
- Albumin: A naturally occurring plasma protein.
- Dextran: A synthetic polysaccharide.
- Hetastarch: A synthetic starch-based colloid.
3. Blood Products: In cases of significant blood loss, blood transfusions are essential. This includes:
- Packed Red Blood Cells (PRBCs): Increase oxygen-carrying capacity.
- Fresh Frozen Plasma (FFP): Replaces clotting factors.
- Platelets: Essential for coagulation.
Determining the Dose: A Multifaceted Approach
The dose of any volume expander is not a fixed number. It depends critically on several factors:
1. Assessment of Fluid Deficit
Accurate assessment is paramount. This involves:
- Clinical evaluation: Assessing the patient's vital signs (heart rate, blood pressure, respiratory rate), level of consciousness, skin perfusion (capillary refill time), urine output, and overall clinical appearance.
- Laboratory tests: Hemoglobin and hematocrit levels provide insights into the severity of blood loss. Electrolyte levels help guide fluid choices.
- Estimating blood loss: This can be challenging, particularly in cases of internal bleeding. Consider the mechanism of injury and any visible signs of blood loss.
2. Type of Volume Expander
The choice of fluid influences dosage. Crystalloids distribute widely, requiring larger volumes to achieve the same intravascular effect as colloids. Colloids stay primarily in the bloodstream, needing less volume but potentially carrying higher risks of adverse effects.
3. Patient-Specific Factors
Individual factors greatly affect dosage:
- Age: Infants and elderly patients require different fluid management strategies due to varying physiological reserve and renal function.
- Pre-existing conditions: Kidney disease, heart failure, and liver disease all influence fluid resuscitation.
- Ongoing fluid losses: Continued bleeding or ongoing fluid loss from diarrhea or vomiting needs continuous replacement.
4. Monitoring Response
Continuous monitoring is vital to gauge the effectiveness of fluid resuscitation and adjust the dosage accordingly:
- Vital signs: Closely observe blood pressure, heart rate, respiratory rate, and urine output.
- Central venous pressure (CVP) or pulmonary artery catheter (PAC): These advanced monitoring techniques provide more precise assessment of fluid status but are not always necessary in all cases.
- Laboratory tests: Repeat hematocrit and electrolyte measurements as needed.
Practical Considerations and Dosage Guidelines (General, Not to be Interpreted as Specific Medical Advice)
While precise dosage calculations depend on the specifics of each case, some general principles can be outlined. These are broad guidelines and should never substitute for professional medical judgment.
Crystalloid Resuscitation
The initial bolus of crystalloid often ranges from 250 mL to 1000 mL for adults, administered rapidly. Subsequent fluid administration depends on the patient's response. In pediatric cases, dosage is calculated based on weight, often starting with 20 mL/kg.
Colloid Resuscitation
Colloids are usually administered in smaller volumes than crystalloids to achieve similar intravascular volume expansion. Typical initial doses may range from 250 mL to 500 mL for adults, but this varies widely depending on the specific colloid and the patient's condition.
Blood Product Resuscitation
Blood product administration is guided by the severity of blood loss and the patient's hematocrit. Transfusion protocols vary depending on the institution, but often involve replacing lost blood volume with PRBCs, FFP, and platelets as needed.
Potential Complications and Adverse Effects
Fluid resuscitation, despite being life-saving, carries potential risks:
- Fluid overload: Excessive fluid administration can lead to pulmonary edema, heart failure, and peripheral edema.
- Electrolyte imbalances: Fluid administration can disrupt electrolyte balance, leading to hyponatremia, hyperkalemia, or hypokalemia.
- Coagulopathy: Dilution of clotting factors by crystalloids can worsen bleeding.
- Allergic reactions: Reactions to colloids or blood products are possible.
- Infection: Blood products carry a risk of transfusion-transmitted infections.
Conclusion: The Importance of Individualized Treatment
Determining the dose of emergency volume expanders is a complex process requiring a thorough understanding of the patient's condition, the type of volume expander used, and continuous monitoring of the patient's response. There is no one-size-fits-all answer; effective fluid resuscitation relies on individualized treatment strategies tailored to each patient's specific needs. This information is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition. The physician or other qualified medical professional must make the final determination regarding appropriate fluid resuscitation strategy and dosage, considering the patient's unique circumstances and continually assessing the response to treatment.
Latest Posts
Latest Posts
-
Exercise 40 Review Sheet Art Labeling Activity 1
May 09, 2025
-
Power Cords Can Be Damaged By Which Of The Following
May 09, 2025
-
Which Settlement Option Pays A Stated Amount To An Annuitant
May 09, 2025
-
Which Of The Following Is An Example Of Potential Energy
May 09, 2025
-
Which Gland Is Not Matched With Its Type Of Secretion
May 09, 2025
Related Post
Thank you for visiting our website which covers about What Is The Dose For Emergency Volume Expander . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.