What Is The Underlying Cause Of Sickle Cell Disease Quizlet
Breaking News Today
Mar 23, 2025 · 6 min read
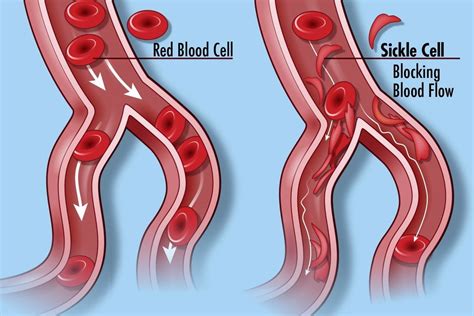
Table of Contents
What is the Underlying Cause of Sickle Cell Disease? A Comprehensive Guide
Sickle cell disease (SCD) is a serious inherited blood disorder that affects millions worldwide. Understanding its underlying cause is crucial for comprehending its symptoms, complications, and the ongoing research into effective treatments. This comprehensive guide delves deep into the genetic and molecular mechanisms that drive this debilitating disease. We'll explore the intricacies of hemoglobin, gene mutations, and the cascade of events leading to the characteristic sickling of red blood cells.
H2: The Role of Hemoglobin: The Oxygen Transporter
At the heart of SCD lies a problem with hemoglobin, the protein responsible for carrying oxygen throughout the body within red blood cells. Healthy red blood cells are flexible and disc-shaped, easily navigating through even the smallest blood vessels. This flexibility is largely dependent on the structure and function of normal hemoglobin (hemoglobin A, or HbA). HbA is a tetramer, meaning it’s composed of four subunits: two alpha (α) and two beta (β) globin chains. Each subunit contains a heme group, which binds to and carries oxygen.
H3: The Sickle Hemoglobin Mutation: A Single Amino Acid Change with Profound Consequences
In individuals with SCD, a single point mutation in the gene encoding the beta-globin chain leads to the production of abnormal hemoglobin S (HbS). This seemingly minor change – the substitution of a single amino acid, valine, for glutamic acid at the sixth position of the beta-globin chain – has profound consequences.
H3: Understanding the Molecular Mechanism of Sickling
The valine substitution alters the surface charge of the beta-globin chain. When deoxygenated, HbS molecules tend to polymerize, or stick together, forming long, rigid fibers within the red blood cells. These fibers distort the cell's shape, causing it to become rigid and sickle-shaped. This sickling process is reversible, meaning the cells can return to their normal shape when oxygen levels are high. However, repeated sickling and unsickling cycles weaken and damage the cell membranes, leading to premature destruction of the red blood cells.
H2: Inheritance Patterns: How SCD is Passed Down
SCD is inherited in an autosomal recessive pattern. This means that both parents must carry the sickle cell gene (HbS) to pass the disease on to their child. There are three possible genotypes resulting from the inheritance of sickle cell genes:
- HbA/HbA (Homozygous Normal): Individuals with two copies of the normal HbA gene are completely healthy and do not have SCD. They do not carry the sickle cell trait.
- HbA/HbS (Heterozygous Carrier): Individuals with one copy of the HbA gene and one copy of the HbS gene are carriers of the sickle cell trait. They typically do not experience symptoms of SCD, but they can pass the HbS gene on to their children. This condition is often referred to as sickle cell trait.
- HbS/HbS (Homozygous Affected): Individuals with two copies of the HbS gene have SCD. They will experience the characteristic symptoms and complications associated with the disease.
H2: The Cascade of Events Leading to SCD Symptoms
The sickling of red blood cells is the primary cause of the many symptoms associated with SCD. These symptoms arise from a complex interplay of factors:
- Vasoocclusion: Sickled red blood cells are rigid and sticky, and they tend to obstruct blood flow in small blood vessels. This blockage, known as vasoocclusion, is responsible for many of the painful crises characteristic of SCD. The pain results from reduced oxygen delivery to tissues and organs.
- Hemolysis: Sickled cells are fragile and break down prematurely in the spleen and other organs. This leads to anemia, a condition characterized by a low number of red blood cells, resulting in fatigue, shortness of breath, and pallor.
- Chronic Organ Damage: Repeated episodes of vasoocclusion and hemolysis can lead to chronic damage to various organs, including the spleen, kidneys, liver, lungs, brain, and bones. This damage can cause a wide range of complications, including stroke, kidney failure, infections, and acute chest syndrome.
H2: Diagnosing Sickle Cell Disease
Diagnosis of SCD involves several methods:
- Newborn Screening: Most developed countries now have newborn screening programs that test for SCD and other inherited metabolic disorders. This early detection is crucial for initiating timely treatment and intervention.
- Hemoglobin Electrophoresis: This laboratory test separates different types of hemoglobin, allowing for the identification of HbS. This is the gold standard for diagnosing SCD.
- DNA Testing: Genetic testing can confirm the diagnosis and determine the specific mutations responsible for SCD.
H2: Treatment and Management of Sickle Cell Disease
The management of SCD is multifaceted and aims to reduce the frequency and severity of painful crises, prevent complications, and improve overall quality of life. Treatment strategies include:
- Hydroxyurea: This medication stimulates the production of fetal hemoglobin (HbF), which does not sickle and can improve blood flow.
- Blood Transfusions: Regular blood transfusions can increase the proportion of healthy red blood cells and reduce the risk of complications.
- Bone Marrow Transplant: For some patients, a bone marrow transplant may be an option to replace the defective bone marrow with healthy cells capable of producing normal hemoglobin.
- Pain Management: Effective pain management is essential for controlling the pain associated with painful crises. This usually involves a combination of medications, including analgesics and other pain-relieving drugs.
- Gene Therapy: Recent advances in gene therapy hold promise for long-term treatment and even a potential cure for SCD.
H2: The Future of Sickle Cell Disease Research
Research on SCD continues to advance rapidly, focusing on developing new and improved treatments, including gene editing techniques such as CRISPR-Cas9, which offer the potential to correct the underlying genetic defect in individuals with SCD. These advancements bring hope for a future where SCD is no longer a life-threatening disease but a manageable condition.
H2: Addressing Misconceptions about Sickle Cell Disease
It's important to clarify some common misconceptions about SCD:
- Sickle cell trait is not the same as sickle cell disease: Individuals with the sickle cell trait do not typically experience symptoms of the disease but can pass the gene onto their children.
- SCD is not contagious: It is an inherited genetic disorder and cannot be spread from one person to another.
- SCD is not solely a disease affecting African Americans: While it is more prevalent in populations with origins in Africa, the Middle East, and the Mediterranean, it can affect individuals of any ethnicity.
H2: The Importance of Awareness and Support
Raising awareness about SCD is critical for early diagnosis, access to appropriate care, and reducing the stigma associated with the disease. Supporting organizations dedicated to SCD research and patient care plays a vital role in improving the lives of those affected by this challenging condition.
H2: Conclusion: A Multifaceted Disease Requiring a Multifaceted Approach
The underlying cause of sickle cell disease is a single point mutation in the beta-globin gene leading to the production of abnormal HbS, causing red blood cells to sickle and leading to a cascade of complications. Understanding this genetic basis, the intricate molecular mechanisms, and the subsequent physiological consequences is crucial for developing effective treatments and improving the lives of those affected by this inherited blood disorder. Ongoing research offers hope for future breakthroughs, highlighting the importance of continued efforts towards prevention, early diagnosis, and comprehensive management of this complex and debilitating disease. The future of SCD management is bright, promising improved treatments and a better quality of life for those living with this condition. Continued research, education, and support are essential to ensure progress towards a future where SCD is manageable and its impact minimized.
Latest Posts
Latest Posts
-
The Capacity For Emergency Management And Response Personnel To Interact
Mar 24, 2025
-
Name The Specific Feature Indicated In The Figure
Mar 24, 2025
-
Yo Hablo Espanol No Hablo Ingles
Mar 24, 2025
-
Sunlight Is Slowed Most When Traveling Through
Mar 24, 2025
-
Identify Elements Of Article Ii Of The Code Of Conduct
Mar 24, 2025
Related Post
Thank you for visiting our website which covers about What Is The Underlying Cause Of Sickle Cell Disease Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
