When Communicating With A Visually Impaired Patient You Should
Breaking News Today
Mar 12, 2025 · 6 min read
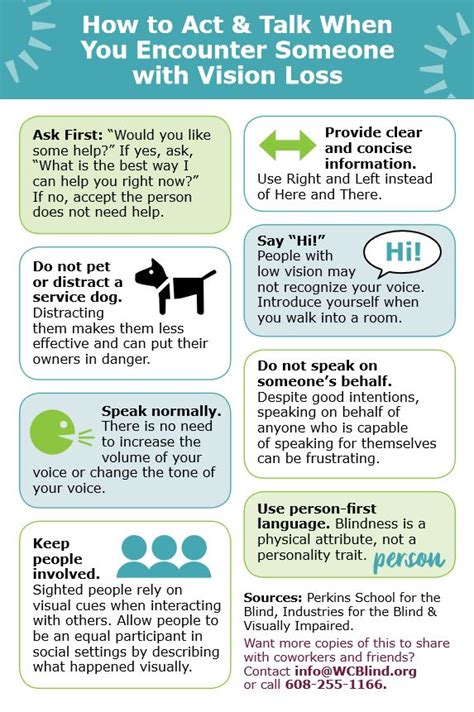
Table of Contents
Communicating Effectively with Visually Impaired Patients: A Comprehensive Guide
Effective communication is crucial in healthcare, and it takes on even greater significance when interacting with visually impaired patients. Misunderstandings can lead to decreased patient satisfaction, compromised care, and even medical errors. This comprehensive guide explores essential strategies for communicating effectively with visually impaired individuals, ensuring they feel respected, understood, and actively involved in their healthcare journey.
Understanding Visual Impairments: A Spectrum of Needs
Before diving into communication techniques, it's crucial to acknowledge the diverse nature of visual impairments. The term "visually impaired" encompasses a wide range of conditions, from low vision (where some sight remains) to total blindness. The level of impairment significantly impacts communication needs. Someone with low vision might benefit from large print materials, while someone with total blindness will rely entirely on other senses. Never assume the extent of a patient's visual impairment. Always ask politely and directly about their visual abilities and preferred communication methods.
Types of Visual Impairments and Communication Considerations:
- Low Vision: Individuals with low vision may still be able to see some details, but may struggle with reading small print or recognizing faces at a distance. They may benefit from larger print materials, good lighting, and clear, concise verbal instructions.
- Legal Blindness: This typically refers to a visual acuity of 20/200 or worse in the better eye with correction, or a visual field of 20 degrees or less. These individuals often rely heavily on assistive technology and verbal communication.
- Total Blindness: Individuals with total blindness have no light perception. They rely entirely on auditory and tactile communication methods.
Essential Communication Strategies: Building a Bridge of Understanding
Effective communication with visually impaired patients involves more than just speaking clearly. It's about creating an inclusive and welcoming environment where they feel comfortable and empowered.
1. Verbal Communication: The Foundation of Connection
- Introduce Yourself Clearly: Begin by identifying yourself and your role. State your name and title explicitly. This sets a foundation of trust and establishes your presence.
- Speak Directly to the Patient: Avoid talking around the patient or to their companion. Address them directly, using their name if you know it.
- Use Clear and Concise Language: Avoid jargon, metaphors, and complex sentence structures. Use simple, direct language that is easy to understand.
- Maintain a Normal Tone of Voice: Don't raise or lower your voice unnecessarily. A natural tone conveys respect and avoids making the patient feel patronized.
- Describe the Environment: Provide spatial orientation by describing the layout of the room, the location of objects, and the direction of movement. For instance, "The examination table is directly in front of you, about three feet away."
- Use Tactile Aids: Consider using tangible objects to illustrate points or provide sensory information. For example, using a model of an organ or a textured sample to describe a condition.
2. Non-Verbal Communication: The Unspoken Language
- Announce Your Presence: Before touching the patient, verbally announce your presence and your intention. For example, "I'm going to take your blood pressure now."
- Use Tactile Cues: Offer your arm or hand for the patient to guide themselves. This allows for safe movement and reduces anxiety.
- Maintain Appropriate Personal Space: Respect the patient's personal space, as they might be sensitive to unexpected touch.
- Be Mindful of Body Language: Maintain open and inviting body language, making eye contact if appropriate. For those who are blind, eye contact may not be as important as your tone of voice and clear communication.
- Listen Actively: Pay attention to what the patient is saying, both verbally and non-verbally. Show genuine interest and empathy.
3. Utilizing Assistive Technology and Sensory Aids
- Describe Visual Aids: If using visual aids like charts or diagrams, describe them in detail. Offer alternative formats like tactile diagrams or audio descriptions.
- Use Magnifiers or Large Print Materials: Provide materials in larger fonts or use magnifiers if the patient has low vision.
- Screen Readers and Voice Recognition Software: For patients who use these technologies, learn how they operate to ensure smooth and efficient communication.
- Audio Descriptions and Podcasts: Utilize audio resources to provide patient education and important information.
4. Involving Family and Support Systems
- Respect Patient Privacy: While family members may offer support, always ensure you communicate directly with the patient, respecting their privacy and autonomy.
- Engage Family in Communication Strategy: If the patient agrees, involve family members in understanding their communication needs and preferences. They can help relay information and ensure clarity.
5. Patience and Empathy: The Cornerstones of Effective Care
- Allow Extra Time: Communication with visually impaired patients may take longer, so allow extra time for conversations and explanations.
- Be Patient and Understanding: Show patience with any challenges in communication and be understanding of the patient's experience.
- Emphasize Empowerment: Encourage the patient's active participation in their healthcare decisions. Provide information in a way that allows them to make informed choices.
Specific Communication Scenarios: Navigating Healthcare Encounters
Let's delve into specific healthcare encounters and how to adapt communication strategies for optimal effectiveness.
During a Physical Examination:
- Explain Each Step Clearly: Before touching the patient, announce what you are going to do and why. For instance, "I'm going to check your pulse now by placing my fingers on your wrist."
- Provide Tactile Feedback: Explain findings using tactile cues where appropriate. For example, when palpating an abdomen, describe the texture and any abnormalities.
- Use Descriptive Language: Replace visual descriptions with auditory and tactile ones. For example, instead of saying "your skin looks pale," say "your skin feels cool to the touch."
During Patient Education:
- Use Multiple Sensory Modalities: Employ both verbal explanations and tangible aids to enhance understanding.
- Provide Information in Accessible Formats: Offer materials in Braille, large print, or audio formats.
- Confirm Understanding: Ask open-ended questions to assess the patient's understanding of the information. Avoid simply asking if they understood.
During Medication Instruction:
- Describe Medication Clearly: Provide detailed information about each medication, including its purpose, dosage, and administration instructions.
- Utilize Tactile Cues for Identification: If medication containers are similar, use tactile markers to help distinguish them.
- Confirm Understanding Through Repetition: Have the patient repeat the instructions back to ensure they are clear.
Addressing Concerns and Anxiety:
- Create a Safe Space: Ensure the environment is safe and comfortable for the patient.
- Validate Their Feelings: Acknowledge and validate any concerns or anxieties the patient may express.
- Offer Reassurance: Provide reassurance and support throughout the interaction.
Beyond the Clinical Setting: Expanding Accessibility
Effective communication extends beyond the hospital or clinic. Healthcare professionals should advocate for accessibility in all healthcare settings, ensuring visually impaired individuals can navigate and access information independently. This includes:
- Accessible Websites and Online Resources: Healthcare websites should be designed with accessibility features for visually impaired users, such as screen reader compatibility.
- Accessible Forms and Documents: Patient intake forms and other documents should be available in accessible formats, such as Braille or large print.
- Accessible Signage and Wayfinding: Hospitals and clinics should have clear and accessible signage and wayfinding systems.
Conclusion: Empowering Through Effective Communication
Communicating effectively with visually impaired patients requires a shift in perspective, moving beyond simply providing information to fostering a genuine connection built on trust and respect. By incorporating the strategies outlined in this guide, healthcare professionals can create an inclusive and empowering environment where visually impaired individuals feel understood, respected, and actively involved in their own care. Remember, effective communication is not just a skill; it is a fundamental aspect of providing compassionate and high-quality healthcare to all patients.
Latest Posts
Latest Posts
-
Carmen And Maria Are Studious In Spanish
May 09, 2025
-
The Overall Function Of The Calvin Cycle Is
May 09, 2025
-
Resting Your Foot On The Brake Pedal Is Called
May 09, 2025
-
A Disinfectant Is Used On Your Work Surface
May 09, 2025
-
The Kub Examination Looks For Defects In The
May 09, 2025
Related Post
Thank you for visiting our website which covers about When Communicating With A Visually Impaired Patient You Should . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.