When Is The Placement Of An Endotracheal Tube Recommended
Breaking News Today
Mar 30, 2025 · 5 min read
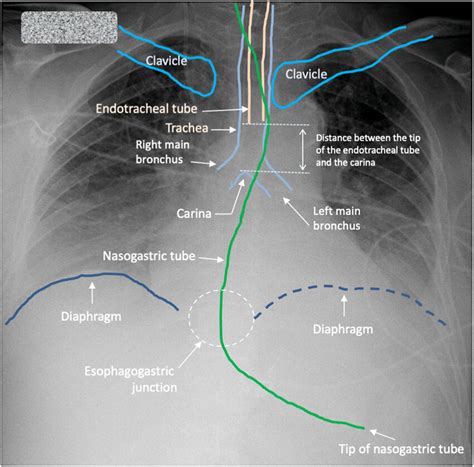
Table of Contents
When is Placement of an Endotracheal Tube Recommended?
Endotracheal intubation, the insertion of a tube into the trachea (windpipe) to secure an airway, is a critical procedure in modern medicine. It's not a decision taken lightly; it requires careful consideration of the patient's condition and the potential risks involved. This comprehensive guide delves into the various clinical scenarios where endotracheal tube placement is recommended, emphasizing the importance of appropriate patient assessment and the potential complications.
Understanding the Need for Endotracheal Intubation
The primary goal of endotracheal intubation is to establish and maintain a patent airway. This means ensuring a clear and unobstructed passage for air to travel to and from the lungs. When a patient is unable to maintain their own airway adequately, or when there's a high risk of airway compromise, intubation becomes necessary.
Situations Requiring Immediate Intubation
Some situations demand immediate intervention, making endotracheal intubation a life-saving procedure. These include:
-
Respiratory Failure: This is a state where the lungs are unable to adequately exchange oxygen and carbon dioxide, leading to dangerously low oxygen levels (hypoxemia) and high carbon dioxide levels (hypercapnia). Symptoms may include labored breathing, cyanosis (bluish discoloration of the skin), altered mental status, and decreased oxygen saturation levels.
-
Apnea: Complete cessation of breathing, requiring immediate intervention to prevent death.
-
Cardiac Arrest: During cardiac arrest, effective ventilation is crucial. Intubation provides a secure airway for delivering oxygen and assisting ventilation.
-
Severe Upper Airway Obstruction: Conditions such as epiglottitis, laryngeal edema, or severe trauma to the face or neck can obstruct the airway, making breathing impossible. Immediate intubation is necessary to bypass the obstruction.
-
Trauma with Potential Airway Compromise: Patients with severe facial or head trauma are at significant risk of airway obstruction due to swelling, bleeding, or bone fragments. Prophylactic intubation might be considered to prevent potential complications.
-
Expected Difficult Airway: In certain situations, the anatomy of a patient’s airway might make intubation challenging. This may be due to obesity, craniofacial abnormalities, or previous neck surgery. Preemptive intubation might be chosen to avoid a potentially life-threatening situation.
-
Loss of Protective Reflexes: Patients with decreased levels of consciousness, such as those in a coma or under deep sedation, may lose their gag and cough reflexes, increasing the risk of aspiration (inhalation of food, fluids, or vomit into the lungs). Intubation safeguards against aspiration.
Situations Requiring Elective Intubation
In contrast to immediate intubation, which is life-saving, elective intubation is planned in advance to support ventilation and oxygenation. These situations include:
-
Preoperative Intubation: Certain surgical procedures, particularly those involving the chest, abdomen, or head and neck, may require controlled ventilation during surgery. Intubation allows for precise control of ventilation and oxygenation.
-
Prolonged Mechanical Ventilation: Patients with severe lung disease, such as pneumonia, acute respiratory distress syndrome (ARDS), or chronic obstructive pulmonary disease (COPD) exacerbations, might require prolonged mechanical ventilation to support breathing.
-
Postoperative Management: Following major surgery, especially thoracic or abdominal surgery, patients may experience respiratory depression or compromised breathing. Intubation helps in managing pain, reducing risk of aspiration and promoting adequate oxygenation.
Assessing the Need for Intubation
The decision to intubate is never taken lightly. A thorough assessment is crucial, incorporating several factors:
-
Airway Assessment: The physician evaluates the patient's airway for any anatomical abnormalities, the presence of secretions, and the patient's ability to protect their airway. The Mallampati score, thyromental distance, and other clinical indicators help assess the difficulty of intubation.
-
Respiratory Assessment: This includes monitoring respiratory rate, depth, effort, and oxygen saturation levels. Blood gas analysis helps determine the severity of respiratory compromise.
-
Neurological Assessment: The patient's level of consciousness, Glasgow Coma Scale score, and pupillary response are important indicators of neurological status and the potential need for airway support.
-
Cardiovascular Assessment: Heart rate, blood pressure, and rhythm are monitored to assess the patient's overall cardiovascular status.
Potential Complications of Endotracheal Intubation
While endotracheal intubation is a life-saving procedure, it carries potential complications:
-
Hypoxemia: Low blood oxygen levels can occur during or after intubation if the procedure is not performed correctly or if the tube is misplaced.
-
Hypercapnia: Elevated carbon dioxide levels in the blood can occur due to inadequate ventilation.
-
Trauma to the airway: Teeth, lips, gums, and vocal cords can be injured during the procedure.
-
Esophageal intubation: Accidental placement of the tube into the esophagus instead of the trachea can lead to serious consequences.
-
Infection: Intubation increases the risk of respiratory infections such as pneumonia.
-
Tube malposition: Incorrect placement of the tube can obstruct airflow or lead to lung collapse.
-
Airway bleeding: Bleeding can occur during the procedure or afterwards.
-
Vocal cord injury: Injury to the vocal cords can lead to voice changes or hoarseness.
Alternatives to Endotracheal Intubation
While endotracheal intubation is often the preferred method for securing an airway, alternatives exist, especially in less urgent scenarios:
-
Non-invasive ventilation (NIV): Techniques like CPAP (continuous positive airway pressure) or BiPAP (bilevel positive airway pressure) can provide respiratory support without the need for intubation.
-
Supraglottic airway devices: These devices provide a pathway for ventilation without the need for endotracheal intubation. Examples include the laryngeal mask airway (LMA) and i-gel.
Conclusion
The decision to place an endotracheal tube is complex and depends on a variety of factors. It is a crucial procedure used to manage life-threatening conditions involving respiratory distress or the inability to protect one's airway. While extremely effective, it's crucial to recognize the potential risks and to consider alternative methods when appropriate. The success of endotracheal intubation relies heavily on careful patient assessment, skilled technique, and ongoing monitoring. The ultimate goal is always to optimize patient care while minimizing potential complications. It's imperative to remember that this information is for educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Latest Posts
Latest Posts
-
Learning To Make Time An Ally Means
Apr 01, 2025
-
The Newest Hvacr Control Systems Operate By
Apr 01, 2025
-
Connective Tissue Covering A Bundle Of Muscle Fibers
Apr 01, 2025
-
Create A Space Large Enough To Give You To Maneuver
Apr 01, 2025
-
Many Jacks Use Hydraulic Power True False
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about When Is The Placement Of An Endotracheal Tube Recommended . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
