Which Action Is The Function Of Antidiuretic Hormone Quizlet
Breaking News Today
Mar 24, 2025 · 6 min read
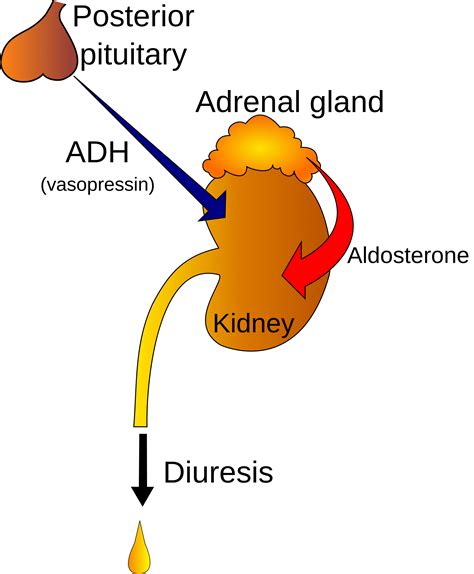
Table of Contents
The Crucial Role of Antidiuretic Hormone (ADH): A Deep Dive into its Actions
Antidiuretic hormone (ADH), also known as vasopressin, is a crucial hormone produced by the hypothalamus and stored in the posterior pituitary gland. Its primary function revolves around maintaining fluid balance in the body, primarily by regulating water reabsorption in the kidneys. Understanding the precise actions of ADH is vital for comprehending various physiological processes and diagnosing related disorders. This comprehensive guide will explore the multifaceted functions of ADH, delving into its mechanisms of action, regulation, and clinical implications.
The Primary Action: Water Reabsorption in the Kidneys
The most well-known action of ADH is its ability to increase water reabsorption in the distal convoluted tubules and collecting ducts of the nephrons in the kidneys. This process is essential for preventing excessive water loss in the urine and maintaining blood volume and osmolality (concentration of solutes in the blood).
Mechanism of Action:
-
Binding to V2 Receptors: ADH reaches the kidneys via the bloodstream and binds to specific V2 receptors located on the basolateral membrane of the principal cells in the collecting ducts.
-
Activation of Adenylyl Cyclase: This binding activates adenylyl cyclase, an enzyme that converts ATP into cyclic AMP (cAMP), a second messenger.
-
cAMP-mediated Protein Kinase A Activation: The increase in cAMP activates protein kinase A (PKA).
-
Aquaporin-2 Insertion: PKA triggers the translocation and insertion of aquaporin-2 (AQP2) water channels into the apical membrane of the principal cells. These channels are water-selective pores that allow water to move from the tubular lumen into the cell.
-
Water Movement: Water then passively moves across the apical membrane via AQP2 channels and subsequently across the basolateral membrane via other aquaporins (AQP3 and AQP4) into the interstitial fluid and eventually into the bloodstream.
Outcome: Increased water reabsorption leads to a decrease in urine volume and an increase in urine concentration (osmolality). This is crucial for maintaining blood pressure and preventing dehydration.
Secondary Actions of ADH: Beyond Water Reabsorption
While water reabsorption is ADH's primary function, it also plays a role in other physiological processes:
1. Vasoconstriction: ADH, at high concentrations, can bind to V1 receptors on vascular smooth muscle cells, leading to vasoconstriction (narrowing of blood vessels). This effect contributes to the maintenance of blood pressure, particularly in situations of hypovolemia (low blood volume). This vasoconstricting effect is less significant than its role in water reabsorption.
2. Platelet Aggregation: ADH can also promote platelet aggregation, contributing to hemostasis (blood clotting). This action, however, is primarily observed at high concentrations and is less significant compared to its effects on the kidneys.
3. Central Nervous System Effects: Some studies suggest that ADH might play a role in certain aspects of central nervous system function, including memory and mood regulation. However, the precise mechanisms and clinical significance of these effects remain to be fully elucidated.
Regulation of ADH Secretion:
The secretion of ADH is tightly regulated by several factors:
1. Osmoreceptors: Osmoreceptors, specialized neurons in the hypothalamus, monitor the osmolality of the blood. An increase in blood osmolality (dehydration) stimulates ADH release, while a decrease inhibits it. This is the primary mechanism regulating ADH secretion.
2. Baroreceptors: Baroreceptors, located in the heart and blood vessels, detect changes in blood pressure. A decrease in blood pressure (hypovolemia) stimulates ADH release, whereas an increase inhibits it.
3. Angiotensin II: Angiotensin II, a potent vasoconstrictor produced during the renin-angiotensin-aldosterone system activation, stimulates ADH release. This is particularly important in maintaining blood pressure during hypovolemia.
4. Stress and Pain: Stressful situations and pain can also stimulate ADH release, possibly through the activation of the sympathetic nervous system.
5. Nausea and Vomiting: Nausea and vomiting can stimulate ADH secretion, possibly due to dehydration or alterations in blood volume.
6. Medications: Some medications can influence ADH secretion. For example, certain antidepressants and chemotherapy drugs can affect ADH levels.
Clinical Significance of ADH Dysregulation:
Disruptions in ADH secretion or action can lead to several clinical conditions:
1. Diabetes Insipidus (DI): DI is characterized by the inability to concentrate urine due to insufficient ADH secretion (central DI) or impaired renal response to ADH (nephrogenic DI). Symptoms include polyuria (excessive urination), polydipsia (excessive thirst), and dehydration.
2. Syndrome of Inappropriate Antidiuretic Hormone (SIADH): SIADH is characterized by excessive ADH secretion, leading to fluid retention, hyponatremia (low sodium levels in the blood), and potentially neurological symptoms such as confusion, seizures, and coma.
3. Hypovolemic Shock: In severe cases of hypovolemia (e.g., due to hemorrhage), ADH release can be significantly elevated, contributing to vasoconstriction and attempts to maintain blood pressure. However, if the hypovolemia is severe, these compensatory mechanisms might be insufficient.
Diagnostic Tests for ADH Related Disorders:
Several tests are available to assess ADH function and diagnose related disorders:
- Urine Osmolality and Specific Gravity: These tests help determine the ability of the kidneys to concentrate urine, which is crucial in assessing ADH function.
- Blood Osmolality and Sodium Levels: These tests help detect electrolyte imbalances associated with ADH dysregulation, such as hyponatremia in SIADH.
- Water Deprivation Test: This test involves restricting fluid intake to assess the body's ability to concentrate urine, providing insight into ADH function.
- ADH Stimulation Test: This involves administering exogenous ADH to evaluate the kidneys' response, helping distinguish central DI from nephrogenic DI.
- Copeptin Measurement: Copeptin is a co-secreted peptide with ADH; measuring copeptin can help assess ADH secretion even when ADH levels are difficult to measure.
Treatment Strategies for ADH Disorders:
Treatment strategies for ADH-related disorders depend on the underlying cause and the severity of symptoms. These may include:
- Fluid Restriction (SIADH): In SIADH, restricting fluid intake is often the first-line treatment to reduce fluid retention and hyponatremia.
- Desmopressin (Central DI): Desmopressin, a synthetic ADH analogue, can be used to replace deficient ADH in central DI.
- Thiazide Diuretics (SIADH): These diuretics can increase sodium excretion and help alleviate hyponatremia in SIADH.
- Sodium Chloride Supplementation (Hyponatremia): Administering sodium chloride may be necessary in severe cases of hyponatremia.
- Addressing Underlying Conditions: Treating underlying conditions such as infections, tumors, or medications that might be contributing to ADH dysregulation is crucial.
Conclusion:
Antidiuretic hormone plays a multifaceted and crucial role in maintaining fluid balance and blood pressure. Its primary function, water reabsorption in the kidneys, is essential for preventing dehydration and maintaining homeostasis. Understanding the intricate mechanisms of ADH action, regulation, and its clinical implications is vital for healthcare professionals in diagnosing and managing various physiological conditions. From the intricacies of aquaporin insertion to the clinical manifestations of ADH dysregulation, this hormone’s influence spans a broad range of physiological and pathological processes, highlighting its critical importance in human health. Further research continues to unveil the nuanced roles of ADH, potentially revealing even more about its significance in health and disease.
Latest Posts
Latest Posts
-
A Partial Bath Includes Washing A Residents
May 12, 2025
-
Which Of The Following Describes A Net Lease
May 12, 2025
-
Nurse Logic 2 0 Knowledge And Clinical Judgment
May 12, 2025
-
Panic Disorder Is Characterized By All Of The Following Except
May 12, 2025
-
Positive Individual Traits Can Be Taught A True B False
May 12, 2025
Related Post
Thank you for visiting our website which covers about Which Action Is The Function Of Antidiuretic Hormone Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.