Which Of The Following Statements Is True Of Osteoarthritis
Breaking News Today
Mar 26, 2025 · 6 min read
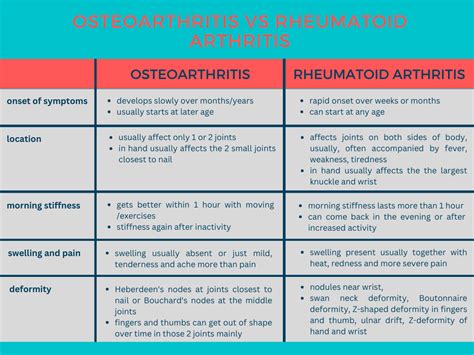
Table of Contents
Which of the Following Statements is True of Osteoarthritis? Understanding the Facts
Osteoarthritis (OA), also known as degenerative joint disease, is the most common form of arthritis. Affecting millions worldwide, it's characterized by the breakdown of cartilage, the cushioning tissue between bones in your joints. While many understand OA involves joint pain, the nuances of the condition often remain unclear. This article will delve deep into common statements about osteoarthritis, clarifying truths and dispelling myths. We'll explore various aspects, from its causes and risk factors to its symptoms, diagnosis, and management.
Understanding Osteoarthritis: Separating Fact from Fiction
Many misconceptions surround osteoarthritis. Let's address some common statements and determine their accuracy:
Statement 1: Osteoarthritis is solely caused by wear and tear.
Partially True. While "wear and tear" plays a significant role, it's an oversimplification. OA isn't simply a matter of joints wearing out over time like a worn-out machine. While aging is a major risk factor, increasing age doesn't automatically mean developing OA. The process is far more complex, involving a breakdown of cartilage, bone remodeling, and inflammation. Genetic predisposition, joint injury, obesity, and repetitive stress all contribute significantly. Therefore, while age-related degeneration contributes, it's not the sole cause.
Statement 2: Osteoarthritis only affects older adults.
False. While OA is more prevalent in older adults (the risk increases significantly after age 40), it can affect people of any age. Young adults and even adolescents can develop OA, particularly if they've experienced previous joint injuries, like a serious knee injury from a sporting accident. Conditions like congenital hip dysplasia can also predispose individuals to early-onset osteoarthritis. This highlights the importance of early diagnosis and management even in younger populations.
Statement 3: Osteoarthritis only affects the weight-bearing joints.
Partially True. OA most commonly affects weight-bearing joints like the knees, hips, and spine. The constant pressure and stress on these joints make them more susceptible to cartilage breakdown. However, OA can also affect other joints, including the hands, feet, and even the neck and shoulders. The smaller joints of the hands are frequently impacted, leading to characteristic bony enlargements known as Heberden's and Bouchard's nodes. This broadens the potential areas affected, emphasizing the systemic nature of the disease.
Statement 4: Osteoarthritis is always accompanied by significant pain.
False. The severity of pain varies significantly among individuals. Some people with advanced OA experience minimal pain, while others suffer from debilitating pain, impacting their daily activities. The presence and intensity of pain are influenced by various factors, including the stage of OA, the location of affected joints, the level of physical activity, and individual pain tolerance. Furthermore, pain management strategies play a crucial role in mitigating the impact of pain.
Statement 5: Osteoarthritis is an inflammatory condition.
Partially True. While not primarily an inflammatory disease like rheumatoid arthritis, OA does involve inflammation. This inflammation occurs as a response to cartilage degradation and the resulting joint damage. The inflammatory process contributes to the pain, swelling, and stiffness experienced by many individuals. While not the primary driver, the inflammatory component is a significant contributing factor to the overall disease progression.
Statement 6: Osteoarthritis is a progressive disease.
True. Osteoarthritis is generally considered a progressive disease, meaning it worsens over time. The cartilage damage gradually accumulates, leading to further joint deterioration, bone spurs (osteophytes), and decreased joint function. However, the rate of progression varies significantly, and many effective interventions can help to slow its advancement. This underscores the importance of proactive management strategies.
Statement 7: There's no cure for osteoarthritis.
True. Currently, there's no cure for osteoarthritis. Treatment focuses on managing symptoms, slowing disease progression, and improving quality of life. This involves a multi-faceted approach, including medication, physical therapy, lifestyle modifications, and in severe cases, surgery. The goal is not necessarily to eliminate the condition but to optimize joint function and reduce pain and disability.
Statement 8: All cases of osteoarthritis require surgery.
False. Surgery is typically considered a last resort for severe cases of osteoarthritis when conservative treatments have failed to provide adequate relief. Many individuals with OA effectively manage their symptoms through lifestyle changes, medication, and physical therapy. Surgical interventions, such as joint replacement, are reserved for those experiencing significant pain and disability despite other treatment options.
Diagnosing Osteoarthritis: A Multifaceted Approach
Diagnosing osteoarthritis relies on a combination of factors:
- Physical Examination: A thorough physical exam will assess joint tenderness, range of motion, swelling, and deformities.
- Medical History: A detailed history of symptoms, including onset, duration, and aggravating factors, is essential. Family history of OA is also relevant.
- Imaging Studies: X-rays are the primary imaging technique used to diagnose OA. They reveal characteristic features such as joint space narrowing, osteophytes, and subchondral sclerosis.
Managing Osteoarthritis: A Holistic Approach
Effective management of osteoarthritis involves a multi-pronged approach:
- Pain Management: Over-the-counter pain relievers (like ibuprofen or acetaminophen) are often used for mild to moderate pain. For more severe pain, stronger medications such as opioids or NSAIDs might be prescribed. However, the risks and benefits of opioid use should be carefully considered with healthcare providers.
- Physical Therapy: Physical therapy plays a crucial role in strengthening surrounding muscles, improving joint mobility, and improving overall function. Therapeutic exercises, customized to each individual’s needs, are beneficial.
- Weight Management: Weight loss is particularly important for individuals with OA of weight-bearing joints as it reduces the stress placed on the joints.
- Lifestyle Modifications: Adapting lifestyle to reduce joint stress is beneficial. This might involve choosing low-impact exercises, using assistive devices, and modifying daily activities.
- Assistive Devices: Canes, walkers, or other assistive devices can help reduce stress on joints and improve mobility.
The Role of Nutrition in Osteoarthritis Management
Nutrition plays a significant role in OA management:
- Anti-inflammatory Diet: A diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help reduce inflammation.
- Vitamin D and Calcium: Adequate intake of Vitamin D and Calcium is crucial for bone health.
- Hydration: Staying well-hydrated is essential for overall joint health.
The Future of Osteoarthritis Treatment
Research continues to advance, leading to promising developments in OA treatment:
- New Medications: Researchers are working on developing new drugs that target specific aspects of the disease process, such as inflammation and cartilage degradation.
- Regenerative Medicine: Innovative approaches, like cartilage regeneration and stem cell therapy, hold the potential to repair damaged cartilage and improve joint function.
Conclusion: A Comprehensive Understanding of Osteoarthritis
Osteoarthritis is a complex condition, and many misconceptions surround it. Understanding the nuances of the disease—from its causes and risk factors to its diagnosis and management—is crucial for effective treatment and improved quality of life. While there's currently no cure, a holistic approach encompassing medication, physical therapy, lifestyle modifications, and nutritional strategies can significantly impact disease progression and improve the lives of those affected. The ongoing research and development in this area offer hope for even better treatments in the future. This article only covers the most prevalent understandings and information surrounding Osteoarthritis. Always consult with your doctor or other healthcare professionals for a proper and personalized diagnosis and treatment plan. Self-treating can be dangerous. Remember to be proactive in your health and seek professional guidance when necessary.
Latest Posts
Latest Posts
-
A Blank Agrees To Help An Immigrant Become A Citizen
Mar 29, 2025
-
Which Of The Following Is Not A Well Known Browser
Mar 29, 2025
-
American Heart Association Cpr Test 25 Questions
Mar 29, 2025
-
Which Action Influences The Abiotic Components Of An Organisms Environment
Mar 29, 2025
-
Which Diet Has The Highest Chance For Symptom Improvement
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Which Of The Following Statements Is True Of Osteoarthritis . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
