Which Type Of Mutation Causes Sickle Cell Anemia Quizlet
Breaking News Today
Mar 23, 2025 · 5 min read
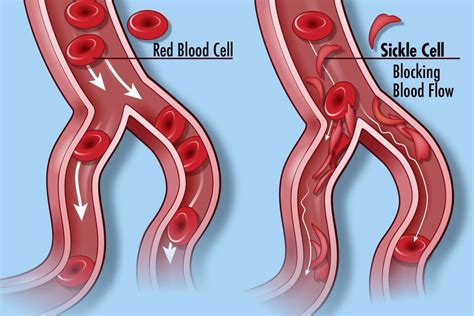
Table of Contents
Which Type of Mutation Causes Sickle Cell Anemia? A Deep Dive
Sickle cell anemia, a debilitating inherited blood disorder, arises from a specific type of genetic mutation. Understanding this mutation is key to comprehending the disease's pathogenesis, symptoms, and potential treatments. This article delves deep into the genetic basis of sickle cell anemia, exploring the precise type of mutation, its consequences at the molecular and cellular levels, and its broader implications for individuals and populations.
The Central Role of the Beta-Globin Gene
Sickle cell anemia is fundamentally a disorder of hemoglobin, the protein responsible for oxygen transport in red blood cells. Hemoglobin is a complex molecule composed of four subunits: two alpha-globin chains and two beta-globin chains. The genetic instructions for producing these chains reside on separate genes.
The culprit in sickle cell anemia lies within the gene responsible for producing the beta-globin chain. This gene, located on chromosome 11, undergoes a specific alteration that leads to the disease's characteristic features.
Point Mutation: The Heart of Sickle Cell Anemia
The defining mutation in sickle cell anemia is a point mutation. This means a single nucleotide base within the DNA sequence of the beta-globin gene is changed. This seemingly small alteration has profound consequences.
Specifically, the mutation involves a change at the sixth codon of the beta-globin gene. The normal codon, GAG, codes for the amino acid glutamic acid. In sickle cell anemia, this codon is mutated to GTG, which codes for the amino acid valine.
This single amino acid substitution – glutamic acid to valine – is the primary cause of sickle cell disease. It might seem trivial, a single change out of hundreds of amino acids, but the effects are dramatic.
Molecular Consequences of the Point Mutation
The substitution of valine for glutamic acid has significant consequences for the hemoglobin molecule's structure and function.
-
Altered Hydrophobicity: Glutamic acid is a negatively charged, hydrophilic (water-loving) amino acid, while valine is a nonpolar, hydrophobic (water-fearing) amino acid. This change alters the surface properties of the beta-globin chain, making it prone to aggregation.
-
Hemoglobin Polymerization: Under low-oxygen conditions, the hydrophobic valine residues on the altered beta-globin chains tend to stick together. This leads to the formation of long, rigid polymers of hemoglobin S (HbS), the abnormal hemoglobin found in individuals with sickle cell anemia.
-
Sickle Cell Shape: These HbS polymers distort the normally flexible, biconcave shape of red blood cells into a characteristic sickle or crescent shape. These misshapen cells are less flexible and more prone to clogging blood vessels.
Cellular and Systemic Effects of Sickled Red Blood Cells
The sickled shape of red blood cells has cascading effects throughout the body:
-
Vascular Occlusion: The rigid, sickle-shaped cells obstruct blood flow in small blood vessels, causing severe pain crises (vaso-occlusive crises). These crises can affect various organs and tissues, including the bones, lungs, spleen, and brain.
-
Hemolysis: Sickled cells are more fragile and prone to premature destruction (hemolysis), leading to anemia. This chronic anemia contributes to fatigue, shortness of breath, and other systemic symptoms.
-
Organ Damage: Repeated episodes of vascular occlusion and hemolysis can damage organs over time, potentially leading to chronic organ dysfunction and failure.
Understanding the Genetics: Inheritance Patterns
Sickle cell anemia is an autosomal recessive disorder. This means an individual must inherit two copies of the mutated beta-globin gene – one from each parent – to develop the disease. Individuals who inherit only one copy of the mutated gene are carriers, meaning they don't exhibit the full-blown disease but can pass on the mutated gene to their children.
This inheritance pattern explains the prevalence of sickle cell anemia in certain populations. In areas where malaria is endemic, carrying one copy of the sickle cell gene offers some protection against malaria, leading to a higher frequency of the sickle cell trait in these populations.
Diagnosis and Management of Sickle Cell Anemia
Diagnosis of sickle cell anemia typically involves genetic testing to identify the specific mutation in the beta-globin gene. This can be done through various methods, including hemoglobin electrophoresis and DNA sequencing.
Management of sickle cell anemia focuses on managing symptoms, preventing complications, and improving quality of life. Treatment approaches may include:
-
Pain Management: Managing pain crises with analgesics and other supportive measures.
-
Hydroxyurea: A medication that stimulates the production of fetal hemoglobin, which does not polymerize and thus helps reduce the severity of symptoms.
-
Blood Transfusions: Providing regular blood transfusions to maintain adequate hemoglobin levels.
-
Bone Marrow Transplant: In some cases, a bone marrow transplant can offer a cure by replacing the affected bone marrow cells with healthy ones.
-
Gene Therapy: Emerging gene therapy approaches aim to correct the underlying genetic defect responsible for sickle cell anemia.
Beyond the Point Mutation: Other Factors
While the point mutation is the primary cause, it's crucial to understand that the severity and manifestations of sickle cell anemia can vary. This variability can be influenced by:
-
Modifier Genes: Other genes can influence the severity of the disease.
-
Environmental Factors: Factors like dehydration, altitude, and infections can trigger pain crises.
-
Genetic Background: An individual's overall genetic makeup can modulate the disease's progression.
The Future of Sickle Cell Anemia Treatment
Research continues to advance our understanding of sickle cell anemia and its management. Innovative therapies, including gene editing technologies like CRISPR-Cas9, hold promise for potential cures. These technologies aim to directly correct the mutated gene in affected individuals, offering a definitive solution to this debilitating disease.
Conclusion: A Single Change, Profound Consequences
The single point mutation in the beta-globin gene, changing GAG to GTG, represents the fundamental cause of sickle cell anemia. This seemingly small change triggers a cascade of molecular, cellular, and systemic effects, leading to the characteristic symptoms and complications of the disease. Understanding this mutation is critical for developing effective diagnostic tools and therapies, ultimately improving the lives of those affected by this inherited disorder. Ongoing research continues to illuminate the intricacies of sickle cell anemia, paving the way for more effective treatments and ultimately, a potential cure. The journey from a single nucleotide change to a complex, life-altering disease highlights the profound power of genetics and the ongoing quest to unravel its mysteries. The continued advancement in genomic technologies, along with a deep understanding of the disease's mechanisms, provides hope for a future where sickle cell anemia is no longer a life-limiting condition.
Latest Posts
Latest Posts
-
Active Resistance Should Be The Immediate Response
Mar 25, 2025
-
The Term Assimilation Is Defined By The Text As
Mar 25, 2025
-
This Statement Is Based On The Assumption That
Mar 25, 2025
-
Fill In The Blanks With The Appropriate Possessive Adjectives
Mar 25, 2025
-
Key Terms Unit 1 And 2 Ap World
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Which Type Of Mutation Causes Sickle Cell Anemia Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
