Why Are Osteocytes Spread Out In Bone Tissue
Breaking News Today
Mar 28, 2025 · 6 min read
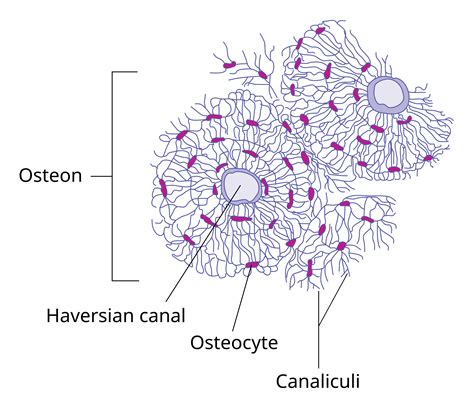
Table of Contents
Why Are Osteocytes Spread Out in Bone Tissue? The Intricate Network of Bone's Living Cells
Bone, often perceived as a static, inert structure, is in fact a remarkably dynamic and living tissue. Its strength and resilience are not solely due to its mineralized matrix, but also to the intricate network of cells embedded within it, primarily osteocytes. Unlike the osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells) found on the bone surface, osteocytes reside within the bone matrix itself, occupying small spaces called lacunae. This dispersed arrangement isn't random; it's a crucial component of bone's functionality, contributing to its strength, remodeling, and overall health. This article will delve into the reasons behind this unique spatial distribution of osteocytes, exploring the mechanisms involved and the implications for bone biology.
The Lacuno-Canalicular Network: Osteocytes' Communication Highway
The key to understanding the dispersed osteocyte network lies in the lacunocanalicular system. Osteocytes reside within lacunae, interconnected by a vast network of tiny canals known as canaliculi. These canaliculi form a complex, three-dimensional system that permeates the bone matrix, allowing for communication and nutrient exchange between osteocytes and the bone surface.
Why the Spaced-Out Arrangement?
The seemingly sparse distribution of osteocytes isn't about inefficiency; rather, it's a highly optimized arrangement serving several critical functions:
-
Mechanical Strength and Stress Sensing: The lacuno-canalicular network acts as a sensor network, detecting mechanical forces applied to the bone. Osteocytes are exquisitely sensitive to mechanical stimuli, such as weight-bearing and muscle contractions. Their dispersed location ensures that the entire bone structure is monitored for stress and strain. This distributed sensing allows for targeted bone remodeling, strengthening areas under high stress and removing bone from areas under less stress. A densely packed arrangement would limit this sensing capability.
-
Efficient Nutrient and Waste Exchange: Osteocytes are metabolically active cells, requiring a constant supply of nutrients and oxygen while producing waste products. The canaliculi facilitate this crucial exchange, allowing nutrients to diffuse from blood vessels in the bone marrow and periosteum to the osteocytes, and vice versa for waste removal. The spread-out arrangement, with its extensive canalicular network, ensures efficient nutrient delivery to even the most distant osteocytes, preventing cell death or compromised function. A more clustered distribution would lead to nutrient limitations and hypoxia in the inner bone regions.
-
Rapid Communication and Coordinated Bone Remodeling: Osteocytes communicate with each other and with cells on the bone surface (osteoblasts and osteoclasts) via the canaliculi. This communication network is crucial for coordinating bone remodeling, a process of continuous bone breakdown and formation that maintains bone strength and integrity. Gap junctions connect adjacent osteocytes, allowing for the rapid transmission of signals, enabling a coordinated response to mechanical stimuli and ensuring efficient remodeling. A clustered arrangement would hinder rapid communication, leading to slower and less efficient bone remodeling.
-
Minimizing Intercellular Interference: Osteocytes, while interconnected, also require a certain degree of separation to maintain their individual functionality and avoid interference. Their dispersed arrangement minimizes this potential interference, ensuring each osteocyte can optimally perform its sensing and signaling roles. Furthermore, this spacing allows for the effective diffusion of signaling molecules, preventing concentration gradients that might confound cellular responses.
-
Adaptation to Bone Microarchitecture: The distribution of osteocytes is also influenced by the bone's microarchitecture. They tend to be more concentrated in areas of high bone turnover and adapt their density based on the local mechanical and metabolic needs. This adaptability ensures that the osteocyte network is always optimized for the specific demands placed on that region of the bone. Understanding this adaptation is key to comprehending how bones respond to changes in loading and to age-related changes.
The Role of Sclerostin and Other Signaling Molecules
Osteocytes play a vital role in regulating bone remodeling through the secretion of various signaling molecules. One particularly important molecule is sclerostin, which inhibits bone formation. The dispersed nature of osteocytes allows for a graded and controlled release of sclerostin, ensuring a fine-tuned regulation of bone remodeling. This nuanced control wouldn't be possible with a densely packed osteocyte population.
Other signaling molecules, including fibroblast growth factors (FGFs), Wnt proteins, and transforming growth factor-beta (TGF-β), are also involved in bone remodeling. The lacuno-canalicular network facilitates the diffusion and precise targeting of these signaling molecules, enabling a well-coordinated and spatially regulated response.
Clinical Implications of Osteocyte Distribution and Function
The spatial distribution and function of osteocytes are crucial for maintaining bone health throughout life. Dysregulation of osteocyte function and connectivity can contribute to various bone diseases, including:
-
Osteoporosis: Characterized by reduced bone mass and increased fracture risk, osteoporosis is often associated with impaired osteocyte function and connectivity. Disruptions to the lacuno-canalicular network can reduce the efficiency of bone remodeling, leading to decreased bone strength.
-
Osteogenesis Imperfecta: Also known as brittle bone disease, osteogenesis imperfecta involves defects in collagen synthesis, leading to fragile and easily fractured bones. This condition can affect osteocyte development and function, leading to further compromised bone quality.
-
Paget's Disease: This bone disorder involves excessive bone turnover, leading to weakened and deformed bones. Disruptions in osteocyte signaling and communication can contribute to the uncontrolled bone remodeling characteristic of Paget's disease.
Understanding the intricate relationship between osteocyte distribution, function, and bone health is crucial for the development of effective treatments and therapies for bone diseases. Research continues to uncover the complexities of osteocyte biology and its implications for bone maintenance and repair.
Future Directions in Osteocyte Research
Ongoing research focuses on several key areas to better understand osteocytes and their role in bone health:
-
Advanced Imaging Techniques: New imaging techniques, such as high-resolution microscopy and advanced synchrotron radiation techniques, are providing unprecedented insights into the three-dimensional architecture of the lacuno-canalicular network and its dynamic changes under various conditions.
-
Mechanobiology of Osteocytes: A deeper understanding of how mechanical forces influence osteocyte function and communication is crucial for developing therapies that promote bone formation and prevent bone loss. This involves sophisticated biomechanical modeling and in vitro studies simulating physiological loading conditions.
-
Osteocyte-Based Therapies: Researchers are exploring the potential of using osteocytes or osteocyte-derived factors in therapies for bone diseases. This includes investigating strategies to stimulate osteocyte function, enhance communication within the lacuno-canalicular network, and promote bone regeneration.
-
The Role of the Extracellular Matrix: The composition and organization of the extracellular matrix surrounding osteocytes influence their function and communication. Research is focused on understanding how changes in the extracellular matrix contribute to bone diseases and how these changes can be targeted for therapeutic interventions.
Conclusion: A Network of Life Within the Bone
The dispersed arrangement of osteocytes within the bone matrix is far from haphazard. It is a meticulously designed network, reflecting the remarkable complexity and adaptability of bone tissue. The lacuno-canalicular system serves as a critical communication highway, enabling nutrient exchange, stress sensing, and the coordinated regulation of bone remodeling. This intricate arrangement is essential for maintaining bone health and ensuring its resilience throughout life. Further research promises to unlock even more secrets of this fascinating cellular network and its crucial role in skeletal health. The spread-out osteocytes are not simply filling space; they are active participants in a dynamic and finely tuned system, a testament to the remarkable sophistication of living bone.
Latest Posts
Latest Posts
-
Blood Cholesterol Levels Can Be Lowered By Quizlet
Mar 31, 2025
-
End Of Life In A Complex Health Situation Edapt Quizlet
Mar 31, 2025
-
The Best Temperature For Short Term Refrigeration Storage Is
Mar 31, 2025
-
The Demand Curve Can Only Shift In One Direction
Mar 31, 2025
-
Explain The Role That Heredity Plays In Skill Related Fitness
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Why Are Osteocytes Spread Out In Bone Tissue . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
