A Patient In Stable Narrow Complex Tachycardia
Breaking News Today
Mar 16, 2025 · 7 min read
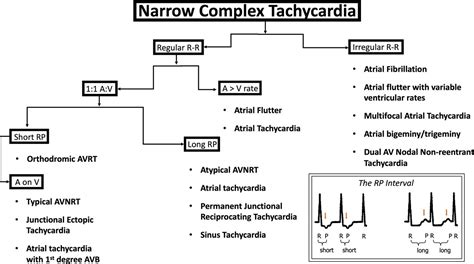
Table of Contents
Stable Narrow Complex Tachycardia: A Comprehensive Guide for Healthcare Professionals
Stable narrow complex tachycardia (NCTS) presents a diagnostic challenge for healthcare providers. Characterized by a rapid heart rate exceeding 100 beats per minute (bpm) with QRS complexes less than 0.12 seconds in duration, and importantly, without signs of hemodynamic instability, NCTS necessitates a systematic approach to diagnosis and management. This comprehensive guide explores the various etiologies, diagnostic workup, and treatment strategies for patients presenting with this condition.
Understanding the Physiology of Narrow Complex Tachycardia
Before delving into the specifics of NCTS, it's crucial to understand the underlying electrophysiological mechanisms. The narrow QRS complex indicates that the tachycardia originates above the ventricles, typically in the atria or atrioventricular (AV) node. This is in contrast to wide complex tachycardias, which originate in the ventricles and have a QRS duration exceeding 0.12 seconds.
The normal conduction pathway involves the sinoatrial (SA) node, initiating the impulse, followed by the atria, AV node, bundle of His, bundle branches, and finally the Purkinje fibers. In NCTS, various disturbances in this pathway can lead to rapid heart rates. These disturbances can include:
-
Supraventricular Tachycardia (SVT): This is a broad term encompassing various arrhythmias originating above the ventricles. The most common causes include atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), and sinus tachycardia.
-
Atrial Flutter: This arrhythmia involves a rapid atrial rhythm typically characterized by “sawtooth” patterns on the ECG. Conduction to the ventricles may be regular or irregular, depending on the AV nodal conduction.
-
Atrial Fibrillation (AF): While often associated with irregular rhythms and wide QRS complexes (especially in the presence of bundle branch block), AF can sometimes present with narrow QRS complexes and a relatively regular ventricular response if the AV node is effectively controlling the ventricular rate.
-
Sinus Tachycardia: While not strictly a tachyarrhythmia, an excessively high sinus rate can mimic NCTS. This is usually caused by physiological stressors like exercise, anxiety, fever, or hypovolemia.
Differentiating Etiologies: A Diagnostic Approach
Diagnosing the underlying cause of NCTS requires a systematic approach combining a thorough history, physical examination, and electrocardiographic (ECG) analysis.
1. History Taking: Crucial Clues
A detailed history is crucial for differentiating potential causes. Important aspects to explore include:
-
Symptom Onset: Sudden versus gradual onset. Sudden onset often suggests arrhythmias like SVT or AF. Gradual onset may indicate conditions like sinus tachycardia due to fever or dehydration.
-
Symptom Duration: The duration of the episode provides valuable information. Prolonged episodes may suggest chronic conditions or structural heart disease.
-
Associated Symptoms: Patients may report palpitations, dizziness, shortness of breath, chest pain, or syncope. These symptoms help assess hemodynamic stability and the severity of the arrhythmia.
-
Medical History: Prior history of cardiac disease, hypertension, hyperthyroidism, or pulmonary embolism should be carefully evaluated.
-
Medications: Certain medications can increase the risk of arrhythmias.
2. Physical Examination: Assessing Hemodynamic Status
The physical examination focuses on assessing hemodynamic stability. This includes:
-
Blood Pressure: Hypotension indicates hemodynamic compromise.
-
Heart Rate and Rhythm: Palpating the carotid pulse can help assess the regularity of the heart rhythm.
-
Lung Sounds: Auscultation for pulmonary edema may suggest cardiac failure.
-
Peripheral Perfusion: Assessing capillary refill time and skin temperature can provide clues about peripheral perfusion.
3. Electrocardiogram (ECG): The Cornerstone of Diagnosis
The ECG remains the cornerstone for diagnosing NCTS. Key features to analyze include:
-
Heart Rate: Accurate determination of the heart rate is crucial.
-
Rhythm: Regularity of the rhythm helps differentiate between various arrhythmias.
-
QRS Complex: Duration and morphology are essential in determining supraventricular versus ventricular origin. A narrow QRS complex (less than 0.12 seconds) strongly suggests a supraventricular origin.
-
P Waves: Analyzing the P waves in relation to the QRS complexes is essential. The presence, absence, or morphology of P waves provides clues to the underlying rhythm. The relationship between P waves and QRS complexes can differentiate between sinus tachycardia, AVNRT, AVRT, atrial flutter, and atrial fibrillation.
-
Other ECG findings: Look for signs of underlying heart disease, such as left ventricular hypertrophy, bundle branch block, or ST-T abnormalities.
4. Further Investigations: When Necessary
Depending on the initial findings, further investigations may be necessary:
-
Electrophysiology Study (EPS): EPS is an invasive procedure used to map the electrical activity of the heart. It's typically indicated in patients with recurrent or symptomatic NCTS to identify the precise mechanism of the arrhythmia and guide ablation therapy.
-
Echocardiogram: An echocardiogram provides detailed information on the structure and function of the heart. It can identify underlying valvular disease, cardiomyopathy, or other structural abnormalities that may contribute to NCTS.
-
Cardiac biomarkers: Troponin levels should be checked if there is any suspicion of myocardial ischemia or infarction.
Management Strategies for Stable Narrow Complex Tachycardia
Management of stable NCTS depends on the underlying etiology, the patient's symptoms, and the presence of any underlying cardiac disease. The primary goals of treatment are to terminate the tachycardia, prevent recurrence, and improve the patient’s quality of life.
1. Vagal Maneuvers: Simple and Non-Invasive
Vagal maneuvers are simple, non-invasive techniques that can be attempted in the initial management of stable NCTS. These maneuvers stimulate the vagus nerve, which can slow the heart rate and potentially terminate the tachycardia. Commonly used maneuvers include:
-
Valsalva maneuver: Forced expiration against a closed glottis.
-
Carotid sinus massage: Gentle massage of the carotid sinus. Caution: This maneuver should only be performed by experienced healthcare professionals due to the potential risk of complications.
-
Cold water immersion: Immersion of the face in cold water.
2. Adenosine: A Pharmacologic Approach
Adenosine is a rapid-acting intravenous medication that can terminate certain types of SVT, particularly AVNRT and AVRT. It works by temporarily blocking AV nodal conduction. However, it's important to note that adenosine is ineffective in other forms of NCTS, such as atrial flutter or atrial fibrillation. Because adenosine has a very short half-life, it's important to be prepared for potential transient side effects, such as chest pain, shortness of breath, and flushing, as they are generally short lived.
3. Other Medications: Beta-blockers and Calcium Channel Blockers
Beta-blockers and calcium channel blockers can be used to slow the heart rate in stable NCTS. These medications are often helpful in managing sinus tachycardia or to control the ventricular rate in atrial fibrillation or atrial flutter. They are typically not first-line treatment for terminating a tachyarrhythmia.
4. Cardioversion: For Unresponsive Cases
Cardioversion is a procedure that uses a synchronized electrical shock to restore a normal heart rhythm. It's typically reserved for cases of NCTS that are unresponsive to medication or vagal maneuvers, or when the patient is hemodynamically unstable.
5. Catheter Ablation: Definitive Treatment
Catheter ablation is a minimally invasive procedure that uses radiofrequency energy to destroy the abnormal electrical pathways that cause NCTS. It is often considered a definitive treatment for recurrent or symptomatic NCTS, particularly AVNRT and AVRT. Ablation is typically recommended after careful consideration and often following an electrophysiology study.
Long-Term Management and Prevention
Long-term management of NCTS depends on the underlying etiology and the patient's response to treatment. Regular follow-up appointments with a cardiologist are crucial for monitoring the patient’s condition and adjusting treatment strategies as needed.
-
Lifestyle Modifications: Lifestyle changes, such as regular exercise, stress reduction techniques, and a healthy diet, can help prevent recurrence in certain cases.
-
Medication Management: Patients may require long-term medication to control their heart rate or prevent recurrence.
-
Regular Monitoring: Regular ECG monitoring and other diagnostic tests may be needed to detect any recurrence or changes in the patient’s condition.
-
Device Therapy: In some cases, patients may benefit from implantable devices, such as pacemakers or implantable cardioverter-defibrillators (ICDs), to control the heart rate or prevent life-threatening arrhythmias.
Conclusion: A Multifaceted Approach
Stable narrow complex tachycardia is a common clinical presentation with diverse underlying causes. A thorough history, physical examination, and ECG analysis are essential for diagnosis. Management strategies range from simple vagal maneuvers to more advanced interventions like cardioversion and catheter ablation. A multifaceted approach, tailored to the individual patient, ensures effective management and improved outcomes. Close collaboration between healthcare providers, regular monitoring, and appropriate patient education are crucial for successful long-term management of NCTS and preventing future episodes. This comprehensive approach will improve patient outcomes and enhance their quality of life.
Latest Posts
Latest Posts
-
The Superficial Temporal Artery Can Be Palpated Quizlet
Mar 18, 2025
-
Rn Comprehensive Online Practice 2023 B With Ngn Quizlet
Mar 18, 2025
-
Administrative Civil Or Criminal Sanctions Cui Quizlet
Mar 18, 2025
-
Sinners In The Hands Of An Angry God Quizlet
Mar 18, 2025
-
Lord Of The Flies Chapter 7 Quizlet
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about A Patient In Stable Narrow Complex Tachycardia . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
