A Patient Is In Refractory Ventricular Fibrillation
Breaking News Today
Mar 13, 2025 · 6 min read
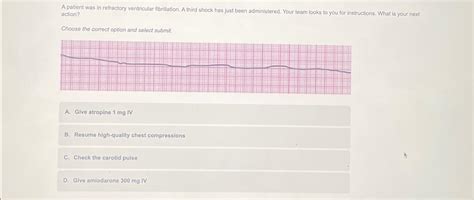
Table of Contents
Refractory Ventricular Fibrillation: A Critical Review
Refractory ventricular fibrillation (VF) represents a life-threatening cardiac arrhythmia characterized by the chaotic electrical activity of the ventricles, resulting in the absence of effective cardiac output. While defibrillation is the cornerstone of VF treatment, refractory VF signifies a failure to achieve return of spontaneous circulation (ROSC) despite multiple attempts at defibrillation and advanced life support (ALS) interventions. This condition carries an extremely high mortality rate, demanding a comprehensive understanding of its pathophysiology, management strategies, and ongoing research avenues.
Understanding the Pathophysiology of Refractory VF
The precise mechanisms underlying refractory VF are complex and multifaceted, often involving a confluence of factors contributing to the sustained electrical instability. Several key contributors include:
1. Myocardial Dysfunction:
- Ischemia: Prolonged myocardial ischemia, whether due to coronary artery disease, myocardial infarction, or other causes, leads to significant cellular damage, electrolyte imbalances, and altered membrane properties. This creates a substrate for sustained arrhythmias. Ischemic myocardium is highly susceptible to re-entrant circuits and disorganized electrical activity, perpetuating VF.
- Myocardial Injury: Acute myocardial injury, particularly in the setting of extensive infarction, can disrupt the coordinated electrical activity of the heart, fostering the development and persistence of VF. The damaged tissue acts as a substrate for re-entrant circuits, making defibrillation less effective.
- Myocardial Stunning: Temporary myocardial dysfunction, even in the absence of significant necrosis, can contribute to refractory VF. This "stunning" effect can be triggered by ischemia, reperfusion injury, or other insults, leading to impaired contractility and increased vulnerability to arrhythmias.
2. Electrolyte Imbalances:
- Hyperkalemia: Elevated serum potassium levels significantly alter myocardial membrane excitability, increasing the likelihood of VF and making it more difficult to terminate. High potassium concentrations prolong the action potential duration and reduce the effective refractory period, facilitating re-entrant circuits.
- Hypokalemia: Conversely, low potassium levels can also destabilize cardiac electrical activity, though typically through different mechanisms.
- Hypocalcemia: Reduced calcium levels can impair myocardial contractility and increase the susceptibility to VF.
- Acidosis: Metabolic acidosis, often seen in severe shock or cardiopulmonary arrest, alters myocardial membrane properties and promotes arrhythmogenesis.
3. Pharmacological Factors:
- Drug Toxicity: Certain medications, including some antidepressants, antiarrhythmics, and other drugs, can contribute to or exacerbate VF. These medications can alter ion channel function, disrupting the normal electrical activity of the heart.
- Drug Interactions: Interactions between multiple drugs can have unpredictable effects on the heart, potentiating the risk of refractory VF.
4. Other Contributing Factors:
- Underlying Heart Disease: Pre-existing conditions such as cardiomyopathy, valvular heart disease, and congenital heart defects can increase susceptibility to VF and make it more refractory to treatment.
- Hypothermia: Hypothermia can significantly alter cardiac electrophysiology, making defibrillation less effective. The slowing of conduction velocity and changes in membrane properties increase the difficulty in terminating VF.
- Tension Pneumothorax: A tension pneumothorax compromises venous return, reducing cardiac output and increasing the likelihood of circulatory collapse and refractory VF.
- Massive Pulmonary Embolism: A large pulmonary embolism can cause acute right heart failure and circulatory collapse, leading to VF that is difficult to treat.
- Cardiac Tamponade: Accumulation of fluid in the pericardial sac impairs diastolic filling, reducing cardiac output and potentially contributing to refractory VF.
Management of Refractory Ventricular Fibrillation: A Multifaceted Approach
The management of refractory VF requires a swift and coordinated effort, employing a stepwise approach that integrates various interventions:
1. High-Quality CPR:
- Chest Compressions: Maintaining high-quality chest compressions is paramount during the resuscitation attempt. Adequate chest compressions ensure some degree of perfusion to vital organs, buying time for other interventions.
- Ventilation: Appropriate ventilation is crucial, maintaining adequate oxygenation and preventing hypercarbia, which can exacerbate myocardial dysfunction.
2. Defibrillation:
- Immediate Defibrillation: Immediate defibrillation is the first-line treatment for VF. Multiple shocks may be necessary, delivered promptly and efficiently according to established guidelines.
- Energy Levels: The energy levels delivered should be in accordance with established guidelines, typically starting with 120-200 Joules for biphasic defibrillators or 360 Joules for monophasic defibrillators, followed by escalating energy levels if necessary.
- Defibrillation Techniques: Proper electrode placement and effective defibrillation technique are critical to maximizing the chances of success.
3. Advanced Life Support (ALS) Medications:
- Epinephrine: Epinephrine is a crucial medication in the treatment of VF, acting as a potent vasoconstrictor and increasing myocardial contractility. It can also increase the effectiveness of defibrillation.
- Vasopressin: Vasopressin, a potent vasoconstrictor, may be considered as an alternative or adjunct to epinephrine.
- Amiodarone: Amiodarone is an antiarrhythmic drug used to suppress ventricular arrhythmias, and may help convert VF to a perfusing rhythm.
- Magnesium Sulfate: Magnesium sulfate is particularly beneficial in cases of VF associated with hypomagnesemia or torsades de pointes.
4. Invasive Hemodynamic Support:
- Intra-Aortic Balloon Pump (IABP): An IABP can improve coronary perfusion pressure and reduce myocardial workload, improving the chances of successful defibrillation.
- Extracorporeal Membrane Oxygenation (ECMO): ECMO can provide temporary circulatory and respiratory support, allowing time for other interventions or recovery. ECMO is particularly useful in cases of refractory VF with severe myocardial dysfunction.
5. Addressing Underlying Causes:
- Treatment of Acidosis: Correcting acidosis with bicarbonate or other appropriate measures is critical in improving myocardial function and defibrillation success.
- Hypothermia Management: Active rewarming may be necessary in cases of hypothermia, as it can improve the effectiveness of defibrillation.
- Tension Pneumothorax Management: Immediate decompression of a tension pneumothorax is crucial.
- Cardiac Tamponade Management: Pericardiocentesis is required to relieve the pressure caused by cardiac tamponade.
- Pulmonary Embolism Management: Treatment of a pulmonary embolism is critical, potentially requiring thrombolysis or other interventions.
- Electrolyte Correction: Addressing electrolyte imbalances, such as hyperkalemia or hypocalcemia, is important for improving myocardial function and responsiveness to defibrillation.
6. Targeted Temperature Management (TTM):
- Induced Hypothermia: After successful ROSC, inducing mild therapeutic hypothermia (32-34°C) has been shown to improve neurological outcomes.
Ongoing Research and Future Directions
Research into refractory VF continues to evolve, with efforts focused on several key areas:
- Improved Defibrillation Techniques: Research is ongoing to improve defibrillation techniques, including the development of new waveform technologies and improved electrode designs.
- Advanced Cardiac Monitoring: Advances in cardiac monitoring technologies allow for more precise identification of the underlying mechanisms of VF, guiding more targeted treatment strategies.
- Pharmacological Interventions: Development of novel antiarrhythmic drugs with improved efficacy and fewer side effects is an area of active investigation.
- Biomarkers: Identifying specific biomarkers that can predict the likelihood of refractory VF could allow for earlier and more targeted interventions.
- Gene Therapy: Gene therapy offers a promising approach for correcting genetic defects that predispose to VF.
- Regenerative Medicine: Research in regenerative medicine explores the possibility of repairing damaged cardiac tissue to reduce the risk of refractory VF.
Conclusion
Refractory ventricular fibrillation remains a significant challenge in emergency medicine and cardiology. While defibrillation remains the cornerstone of treatment, a comprehensive, multi-faceted approach integrating advanced life support, hemodynamic support, and treatment of underlying causes is crucial to improve outcomes. Continued research into improved diagnostic techniques, pharmacological interventions, and novel therapeutic strategies is essential to reduce the mortality associated with this devastating condition. The emphasis should be on prompt recognition, immediate high-quality CPR, and a systematic approach to treatment guided by the latest evidence-based guidelines. The ultimate goal is to improve survival rates and neurological outcomes for patients suffering from refractory ventricular fibrillation.
Latest Posts
Latest Posts
-
Which Of The Following Describes The Probability Distribution Below
May 09, 2025
-
Movement Or Motion Away From The Bodys Midline Is Called
May 09, 2025
-
A Benefit Of A Free Market Can Be That
May 09, 2025
-
Chemical Reactions Form Or Break Between Atoms Ions Or Molecules
May 09, 2025
-
What Is The Size Of The Rc Conf File In Bytes
May 09, 2025
Related Post
Thank you for visiting our website which covers about A Patient Is In Refractory Ventricular Fibrillation . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.