A Patient Is In Refractory Ventricular Fibrillation Quizlet
Breaking News Today
Mar 17, 2025 · 5 min read
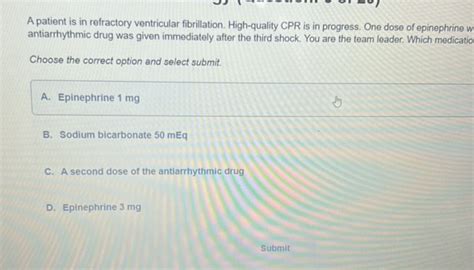
Table of Contents
A Patient in Refractory Ventricular Fibrillation: A Comprehensive Guide
Ventricular fibrillation (VF) is a life-threatening cardiac arrhythmia characterized by chaotic, disorganized electrical activity in the ventricles. This prevents the heart from effectively pumping blood, leading to rapid circulatory collapse and, ultimately, death if not treated immediately. While defibrillation is the primary treatment, a significant challenge arises when VF persists despite repeated attempts at defibrillation – a condition known as refractory ventricular fibrillation (RVF). This article will delve into the complexities of RVF, exploring its causes, management strategies, and prognosis.
Understanding Refractory Ventricular Fibrillation
Refractory ventricular fibrillation is defined as ventricular fibrillation that persists despite at least three attempts at defibrillation with appropriate energy levels (typically 200 joules or more). It represents a critical juncture in resuscitation, demanding immediate and aggressive intervention. The survival rate significantly decreases with each unsuccessful defibrillation attempt, underscoring the urgency of effective management.
Key Characteristics of RVF:
- Persistence despite defibrillation: This is the hallmark characteristic. Despite delivering high-energy shocks, the disorganized electrical activity continues.
- Hemodynamic instability: The lack of effective cardiac output leads to severe hypotension, pulselessness, and absent palpable pulses.
- Rapid deterioration: The patient's condition deteriorates quickly if RVF is not addressed promptly.
- Increased mortality risk: RVF carries a substantially higher mortality risk compared to readily defibrillatable VF.
Causes and Contributing Factors of RVF
RVF is a complex condition with multiple contributing factors that can interplay to make defibrillation ineffective. Understanding these factors is crucial for effective management.
1. Underlying Cardiac Conditions:
- Acute myocardial infarction (AMI): Large anterior wall infarctions, particularly those involving the left anterior descending artery, significantly increase the risk of RVF. The extensive myocardial damage disrupts the electrical conduction pathways, making the heart more susceptible to disorganized rhythms.
- Cardiomyopathy: Conditions like hypertrophic cardiomyopathy, dilated cardiomyopathy, and restrictive cardiomyopathy can predispose individuals to RVF. The structural abnormalities of the heart muscle interfere with normal electrical activity.
- Congenital heart disease: Certain congenital heart defects can increase the risk of arrhythmias, including VF.
- Valvular heart disease: Severe aortic or mitral valve disease can strain the heart, leading to abnormal electrical activity and increased risk of RVF.
2. Electrolyte Imbalances:
- Hyperkalemia: Elevated potassium levels interfere with myocardial repolarization, making the heart more susceptible to arrhythmias, including VF.
- Hypocalcemia: Low calcium levels impair myocardial contractility and can contribute to refractory arrhythmias.
- Hypomagnesemia: Magnesium deficiency can exacerbate arrhythmias, including VF, and hinder the effectiveness of defibrillation.
3. Metabolic Disturbances:
- Acidosis: Metabolic acidosis, often secondary to respiratory or circulatory failure, alters myocardial function and can increase the risk of RVF.
- Hypoxia: Insufficient oxygen supply to the heart muscle impairs its ability to function normally, increasing the susceptibility to arrhythmias.
- Hypothermia: While hypothermia can sometimes slow down arrhythmias, profound hypothermia can also contribute to refractory VF.
4. Drug-Induced Effects:
- Certain medications: Some medications can prolong the QT interval, increasing the risk of Torsades de Pointes, a type of polymorphic ventricular tachycardia that can degenerate into VF.
- Drug toxicity: Overdoses or toxic effects from certain drugs can disrupt cardiac electrical activity.
5. Other Factors:
- Hypovolemia: Severe fluid loss can decrease myocardial perfusion, contributing to refractory arrhythmias.
- Tension pneumothorax: This condition impairs venous return to the heart, reducing cardiac output and increasing the risk of VF.
- Cardiac tamponade: Fluid accumulation in the pericardial sac compresses the heart, hindering its ability to pump blood effectively.
- Pulmonary embolism: A large pulmonary embolism can acutely compromise cardiac function, increasing the risk of VF.
Management of Refractory Ventricular Fibrillation
The management of RVF requires a coordinated and aggressive approach involving multiple interventions. The goal is to restore organized cardiac rhythm and effective circulation as quickly as possible.
1. Advanced Cardiovascular Life Support (ACLS) Protocols:
- High-energy defibrillation: Repeated defibrillation with escalating energy levels (up to 360 joules) should be attempted.
- Chest compressions: High-quality chest compressions are crucial to maintain some degree of circulation during the resuscitation efforts.
- Advanced airway management: Secure an airway through endotracheal intubation or other advanced airway techniques to ensure adequate ventilation.
- Medication administration: Specific medications are used to address underlying causes and improve the chances of successful defibrillation.
2. Medications Used in RVF:
- Amiodarone: A potent antiarrhythmic drug, often used for its effectiveness in treating refractory VF.
- Lidocaine: Another antiarrhythmic drug, sometimes used in conjunction with or as an alternative to amiodarone.
- Magnesium sulfate: Administered to correct magnesium deficiency, which can contribute to refractory VF.
- Bicarbonate: May be used to correct acidosis, which can impair myocardial function.
- Epinephrine: Used to improve myocardial contractility and increase coronary perfusion. However, its role in RVF is controversial and its use is guided by specific clinical scenarios.
3. Addressing Underlying Causes:
- Identification and treatment of the underlying cause: This is crucial for long-term success. For example, if RVF is secondary to an acute MI, immediate reperfusion therapy (e.g., percutaneous coronary intervention) is essential. Electrolyte imbalances should be corrected, and other contributing factors addressed.
- Echocardiography: Essential to assess cardiac function and identify structural abnormalities that may be contributing to the arrhythmia.
- Cardiac catheterization: May be necessary to identify and treat coronary artery disease.
- Laboratory tests: Blood tests should be performed to evaluate electrolytes, blood gases, and other relevant parameters.
4. Advanced Therapeutic Interventions:
- Transvenous pacing: If VF converts to asystole or pulseless electrical activity (PEA), transvenous pacing may be necessary to restore a heartbeat.
- Extracorporeal membrane oxygenation (ECMO): In cases of severe refractory VF, ECMO may provide temporary circulatory and respiratory support, allowing time for other interventions to take effect.
- Implantable cardioverter-defibrillator (ICD): Following successful resuscitation, an ICD may be implanted to prevent future life-threatening arrhythmias.
Prognosis and Outcomes
The prognosis for patients with RVF is grave. The mortality rate is significantly higher compared to readily defibrillatable VF. Even with successful resuscitation, the risk of long-term complications and mortality remains elevated due to underlying cardiac conditions and the severity of the initial event.
Conclusion
Refractory ventricular fibrillation represents a critical medical emergency demanding immediate and aggressive intervention. The successful management of RVF requires a comprehensive understanding of its causes, a coordinated approach to treatment using ACLS protocols and advanced therapies, and prompt identification and treatment of the underlying cardiac pathologies. Early recognition, swift application of advanced life support, and focused attention on correcting contributing factors are essential to improve the chances of survival and minimize long-term complications. This underscores the importance of continued research and improved management strategies for this life-threatening condition. While the prognosis remains challenging, advancements in technology and resuscitation techniques offer hope for improved outcomes in the future. Improved prevention strategies and early recognition are key to improving survival rates.
Latest Posts
Latest Posts
-
Describe The Continuous Nature Of The Physical Fitness Concept
Mar 18, 2025
-
High Levels Of Cholesterol Can First Lead Directly To
Mar 18, 2025
-
True Or False Professional And Technical Communication Is Research Oriented
Mar 18, 2025
-
Which Best Describes The Terrorist Planning Cycle
Mar 18, 2025
-
Cdl Combination Test Questions And Answers Pdf
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about A Patient Is In Refractory Ventricular Fibrillation Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
