A Patients Refusal Of Ems Treatment Must Be
Breaking News Today
Mar 29, 2025 · 6 min read
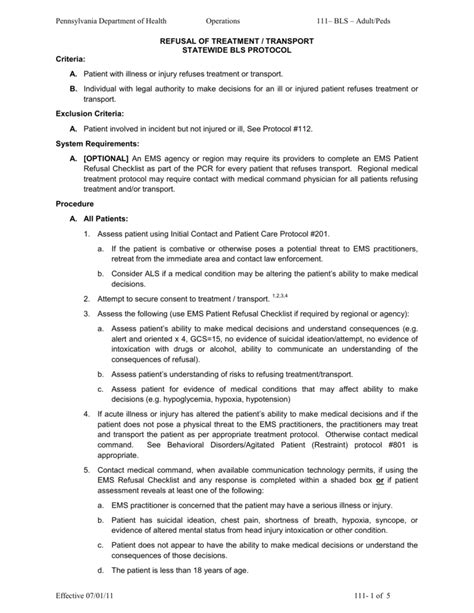
Table of Contents
A Patient's Refusal of EMS Treatment: Understanding the Legal and Ethical Implications
Emergency Medical Services (EMS) personnel face a complex ethical and legal landscape when patients refuse treatment. While the right to refuse medical care is a cornerstone of individual autonomy, ensuring patient safety and upholding legal responsibilities necessitates a nuanced approach. This comprehensive guide delves into the critical aspects of patient refusal of EMS treatment, exploring the legal framework, ethical considerations, documentation procedures, and strategies for effective communication and de-escalation.
Understanding the Legal Right to Refuse Treatment
The foundation of a patient's right to refuse EMS treatment lies in the principle of informed consent. This means a competent adult has the legal authority to make decisions about their own healthcare, including the right to decline medical intervention, even if that decision might seem unwise to others. This right is deeply rooted in common law and is reinforced by numerous state and federal regulations. However, this right is not absolute and comes with certain limitations and considerations.
Key Considerations Limiting the Right to Refuse:
-
Competence: A patient must possess the mental capacity to understand their medical condition, the proposed treatment, and the potential consequences of refusing treatment. Factors such as intoxication, mental illness, or severe cognitive impairment can compromise competence. In such cases, EMS personnel may need to seek alternative legal avenues, such as obtaining consent from a legal guardian or pursuing involuntary commitment if the patient poses a danger to themselves or others.
-
Imminent Danger: If a patient's refusal of treatment poses an immediate and serious threat to their life or health, EMS personnel may have the legal authority to intervene despite the patient's refusal. This is often referred to as the "emergency exception" to informed consent. The threshold for invoking this exception is high and requires a clear and imminent danger to life or limb.
-
Minors: Minors generally lack the legal capacity to refuse medical treatment. Consent must be obtained from a parent or legal guardian. However, there are exceptions, such as mature minors who demonstrate sufficient understanding of their medical condition and treatment options. The age of majority and specific state laws determine the nuances of this situation.
-
Public Safety: While respecting individual autonomy, EMS providers also have a responsibility to ensure public safety. If a patient's refusal of treatment puts others at risk (e.g., a contagious disease), EMS personnel may need to take steps to mitigate that risk, possibly involving public health authorities.
The Ethical Dimensions of Patient Refusal
Beyond the legal framework, the ethical considerations surrounding patient refusal of EMS treatment are profound. EMS providers are bound by ethical obligations to:
-
Respect Patient Autonomy: The patient's right to self-determination should be prioritized whenever possible. Coercion or undue influence should be strictly avoided.
-
Beneficence: EMS providers have a duty to act in the best interests of the patient. This requires careful assessment of the patient's condition and the potential risks and benefits of treatment. Balancing beneficence with respect for autonomy is a constant ethical challenge.
-
Non-Maleficence: EMS providers must avoid causing harm to the patient. This necessitates careful consideration of the potential side effects of treatment and the risks associated with intervention.
-
Justice: Ensuring equitable access to EMS services for all patients, regardless of their socioeconomic status, race, or other factors, is a crucial ethical responsibility.
Documentation: A Critical Element
Meticulous documentation is paramount when a patient refuses EMS treatment. The documentation should be clear, concise, and factual, reflecting the following:
-
Patient Identification: Include the patient's name, date of birth, address, and other relevant identifiers.
-
Time and Location: Record the precise time and location of the incident.
-
Assessment of Patient's Condition: Document the patient's vital signs, chief complaint, and other relevant medical information.
-
Explanation of Treatment Options: Clearly describe the treatment options offered to the patient, including the potential benefits and risks of each.
-
Patient's Understanding: Note the patient's understanding of their condition and the proposed treatment, confirming their mental competence to make an informed decision.
-
Patient's Refusal: Clearly document the patient's refusal of treatment, including their reasons, if any. Use direct quotes whenever possible.
-
Witness Information: If witnesses are present, document their names and contact information.
-
EMS Personnel: Include the names and credentials of all EMS personnel involved.
-
Photographs or Videos (with consent): If appropriate and with the patient's consent, taking photographs or videos can provide valuable documentation.
-
Patient Signature: Obtain the patient's signature on a refusal form, if possible. If the patient is unable to sign, document the reason and obtain signatures from witnesses.
Strategies for Effective Communication and De-escalation
Effective communication is crucial in managing situations where patients refuse EMS treatment. EMS personnel should employ the following strategies:
-
Active Listening: Pay close attention to the patient's concerns and fears, allowing them to express themselves fully.
-
Empathy and Respect: Treat the patient with dignity and respect, even if you disagree with their decision.
-
Clear and Concise Explanation: Explain the patient's condition, treatment options, and potential consequences in simple, understandable terms.
-
Answer Questions Thoroughly: Address all of the patient's questions honestly and patiently.
-
Document Everything: Remember, accurate and thorough documentation is crucial in case of future legal issues.
-
De-escalation Techniques: If the patient is agitated or aggressive, use de-escalation techniques to calm them down and create a safe environment. This may involve speaking softly, maintaining a calm demeanor, and offering reassurance.
-
Collaboration with Family and Friends: Involve family members or friends in the decision-making process, if appropriate and if the patient consents.
-
Knowing When to Seek Assistance: If the situation becomes unmanageable, don't hesitate to seek assistance from law enforcement or other relevant authorities. Patient safety and provider safety are paramount.
Consequences of Improper Handling of Refusals
Failure to properly handle a patient's refusal of EMS treatment can have significant legal and ethical consequences, including:
-
Negligence Claims: If the EMS provider fails to properly assess the patient's condition or adequately document the refusal, they may face legal liability for negligence if the patient subsequently suffers harm.
-
Malpractice Suits: Improper handling of a refusal can lead to malpractice lawsuits, particularly if the provider coerced the patient or failed to provide adequate information.
-
Ethical Violations: Failure to respect patient autonomy or to provide appropriate care can lead to disciplinary actions by professional organizations.
-
Reputational Damage: Negative publicity surrounding a mishandled refusal can damage the reputation of the EMS agency and its personnel.
Conclusion: Balancing Autonomy and Responsibility
Navigating a patient's refusal of EMS treatment requires a delicate balance between respecting individual autonomy and fulfilling professional responsibilities. By understanding the legal framework, adhering to ethical principles, maintaining thorough documentation, and utilizing effective communication strategies, EMS personnel can effectively manage these challenging situations while safeguarding both patient safety and legal compliance. Remember, the goal is not to force treatment, but to ensure that the patient makes an informed and autonomous decision, even if that decision involves foregoing medical intervention. The focus should always remain on respectful communication, thorough documentation, and ensuring patient safety within the bounds of the law. When in doubt, consult with supervisors, legal counsel, or other qualified professionals to ensure proper procedures are followed.
Latest Posts
Latest Posts
-
Apoptosis Refers To Cell Death And Quizlet
Mar 31, 2025
-
Debt Consolidation Loans Can Be Used To Quizlet
Mar 31, 2025
-
What Is The Answer To A Division Problem Called
Mar 31, 2025
-
How Many Acres Are In A Section Of Land
Mar 31, 2025
-
Careers In Science Technology Engineering And Mathematics Quizlet
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about A Patients Refusal Of Ems Treatment Must Be . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
