A Persistent Infection Is One In Which
Breaking News Today
Mar 15, 2025 · 6 min read
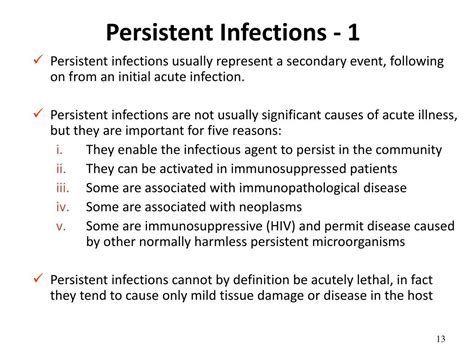
Table of Contents
A Persistent Infection Is One In Which... Understanding Chronic Microbial Challenges
A persistent infection is one in which the infectious agent, whether a virus, bacterium, fungus, or parasite, remains within the host's body for an extended period, often evading the host's immune system and conventional treatment. This isn't simply a delayed clearance of the infection; rather, it represents a complex interplay between the pathogen and the host, leading to a chronic, often low-grade, state of infection. This article will delve into the characteristics of persistent infections, exploring the mechanisms pathogens use to evade the immune system, the consequences of persistent infection, and current approaches to diagnosis and treatment.
Characteristics of Persistent Infections
Persistent infections are characterized by several key features that distinguish them from acute infections:
-
Long duration: Unlike acute infections that resolve within weeks or months, persistent infections can last for years, even decades. This prolonged presence of the pathogen often leads to chronic inflammation and ongoing damage to host tissues.
-
Subclinical or asymptomatic nature: Many persistent infections are asymptomatic or only present with subtle, intermittent symptoms. This makes diagnosis challenging and often leads to delayed treatment, allowing the infection to establish itself firmly.
-
Immune evasion: Persistent pathogens have evolved sophisticated mechanisms to evade detection and destruction by the host's immune system. These mechanisms can involve antigenic variation, immune suppression, latency, and the establishment of intracellular niches.
-
Treatment challenges: The prolonged nature of the infection and the pathogen's ability to evade the immune system often makes treatment difficult. Conventional antimicrobial therapies may be ineffective, requiring long-term or alternative treatment strategies.
-
Potential for reactivation: Some persistent infections, such as those caused by herpesviruses, can enter a latent state where the pathogen's replication is suppressed but the viral genome remains integrated into the host's DNA. This allows for reactivation of the infection under conditions of immune suppression or stress.
Mechanisms of Immune Evasion in Persistent Infections
The ability of persistent pathogens to evade the immune system is a critical factor in their success. Several mechanisms contribute to this immune evasion:
1. Antigenic Variation:
Many pathogens, particularly viruses and some bacteria, undergo antigenic variation, changing the surface antigens they present to the immune system. This prevents the host from mounting an effective immune response because antibodies generated against one antigen may not recognize the altered antigen. Influenza viruses are a classic example, constantly evolving to evade immunity conferred by previous infections or vaccines.
2. Immune Suppression:
Some pathogens directly suppress the host's immune system, either by interfering with immune cell function or by inducing immune tolerance. Human immunodeficiency virus (HIV), for example, specifically targets CD4+ T cells, a critical component of the adaptive immune system, leading to profound immunodeficiency. Epstein-Barr virus (EBV) can also manipulate immune responses to promote its persistence.
3. Latency:
Many viruses, including herpesviruses (e.g., herpes simplex virus, varicella-zoster virus, Epstein-Barr virus), can establish latency. In this state, the viral genome persists in a dormant state within host cells, without producing new viral particles. This prevents the virus from being detected by the immune system, allowing it to persist indefinitely. Reactivation can occur under conditions of immune suppression or stress.
4. Intracellular Persistence:
Some pathogens, such as Mycobacterium tuberculosis, establish intracellular niches within host cells, where they are shielded from the effects of antibodies and other components of the immune system. This protected environment allows the pathogen to persist despite the host's immune response.
Consequences of Persistent Infections
The consequences of persistent infections can vary depending on the specific pathogen and the host's immune status. However, some common consequences include:
-
Chronic inflammation: The continuous presence of the pathogen triggers a persistent inflammatory response, which can lead to tissue damage and organ dysfunction.
-
Increased cancer risk: Certain persistent infections are strongly linked to an increased risk of cancer. For example, chronic infection with hepatitis B or C viruses is a major risk factor for liver cancer, while EBV is linked to several types of lymphomas and nasopharyngeal carcinoma.
-
Autoimmune diseases: In some cases, persistent infections can contribute to the development of autoimmune diseases. Molecular mimicry, where pathogen antigens resemble host antigens, may trigger an autoimmune response targeting host tissues.
-
Impaired immune function: Chronic immune activation and suppression associated with persistent infections can lead to overall impairment of immune function, increasing susceptibility to other infections.
-
Fatigue and other systemic symptoms: Many individuals with persistent infections experience nonspecific symptoms such as fatigue, malaise, and muscle pain. These symptoms can significantly impact quality of life.
Diagnosis of Persistent Infections
Diagnosing persistent infections can be challenging due to their often subtle or asymptomatic nature. Diagnostic approaches often involve a combination of techniques:
-
Serology: Detection of antibodies against the pathogen in the patient's serum can indicate past or present infection. However, the presence of antibodies alone does not always confirm active infection, especially in persistent infections.
-
Molecular techniques: Polymerase chain reaction (PCR) and other molecular methods can detect the pathogen's genetic material directly in clinical specimens, providing more definitive evidence of infection.
-
Culture: Isolation and culture of the pathogen from clinical specimens can confirm the diagnosis and allow for antimicrobial susceptibility testing. However, this is not always successful, especially for fastidious or intracellular pathogens.
-
Imaging techniques: Imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) can identify tissue damage or lesions associated with the infection.
Treatment of Persistent Infections
Treatment of persistent infections is often challenging and requires a multifaceted approach. Strategies may include:
-
Antimicrobial therapy: Antimicrobial drugs, including antibiotics, antivirals, antifungals, and antiparasitics, may be used to target the pathogen. However, the effectiveness of these drugs can be limited by the pathogen's ability to evade the immune system or develop resistance. Long-term therapy may be necessary in some cases.
-
Immune modulation: Modulation of the host's immune response may be used to enhance the clearance of the pathogen. This may involve the use of immunomodulatory drugs or therapies aimed at restoring immune function.
-
Supportive care: Supportive care measures, such as managing symptoms and providing nutritional support, are crucial in improving the patient's quality of life and promoting healing.
-
Novel therapeutic approaches: Researchers are actively exploring novel therapeutic approaches for persistent infections, including new antimicrobial drugs, vaccines, and immunotherapy strategies.
Conclusion
Persistent infections represent a significant challenge to human health, characterized by prolonged duration, immune evasion, and the potential for serious long-term consequences. Understanding the mechanisms by which pathogens establish persistence and evade the immune system is crucial for the development of effective diagnostic and therapeutic strategies. Ongoing research is essential to further unravel the complexities of persistent infections and to improve patient outcomes. The development of novel therapeutic approaches, including targeted therapies and immunotherapies, holds significant promise for the future management of these challenging infections. Further research into the interplay between the pathogen and the host immune response will be critical in advancing our understanding and treatment of these complex conditions. Understanding the intricacies of persistent infections is crucial for developing effective strategies to combat these challenging microbial adversaries.
Latest Posts
Latest Posts
-
What Does The Term Tudor Court Mean
Mar 15, 2025
-
Label The Features Of A Neuromuscular Junction
Mar 15, 2025
-
What Are The 6 Roles Of Political Parties
Mar 15, 2025
-
Es Donde Pones La Cabeza Cuando Duermes
Mar 15, 2025
-
What Is One Way To Begin Saving Startup Capital
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about A Persistent Infection Is One In Which . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
