According To The National Ems Scope Of Practice Model
Breaking News Today
Mar 17, 2025 · 6 min read
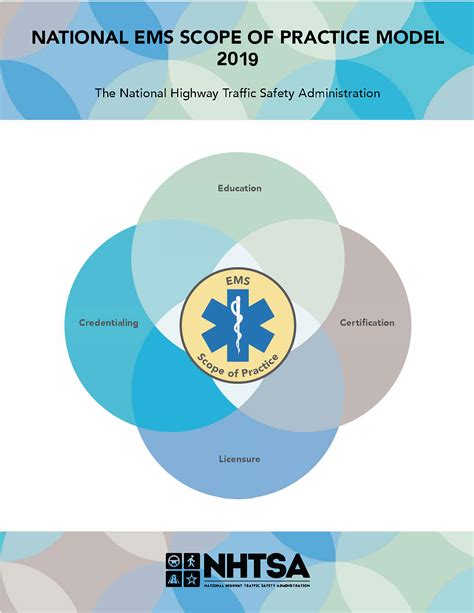
Table of Contents
Understanding the National EMS Scope of Practice Model: A Comprehensive Guide
The National EMS Scope of Practice Model serves as a crucial guideline for Emergency Medical Services (EMS) providers across the United States. It outlines the range of medical services that different levels of EMS personnel—Emergency Medical Responders (EMRs), Emergency Medical Technicians (EMTs), Advanced EMTs (AEMTs), and Paramedics—are permitted to perform. This model, while not legally binding in itself, profoundly influences state-level regulations and sets a benchmark for EMS education and practice. Understanding its intricacies is vital for EMS professionals, educators, and policymakers alike. This comprehensive guide will delve into the key aspects of the National EMS Scope of Practice Model, examining its structure, implications, and future trends.
The Hierarchical Structure of the National EMS Scope of Practice Model
The model employs a tiered system, clearly defining the responsibilities and capabilities of each EMS provider level. This hierarchical structure ensures a progressive increase in complexity and autonomy as providers advance through their training and certification.
Emergency Medical Responder (EMR)
EMRs represent the entry-level in prehospital care. Their scope of practice is generally limited to basic life support (BLS) interventions. This typically includes:
- Assessing the scene: Identifying hazards and ensuring scene safety.
- Basic airway management: Opening the airway using techniques like head tilt-chin lift or jaw thrust.
- CPR and ventilation: Administering cardiopulmonary resuscitation (CPR) and providing rescue breaths using bag-valve masks (BVMs).
- Bleeding control: Applying direct pressure to control external bleeding.
- Emergency splinting: Stabilizing suspected fractures with basic splinting techniques.
- Patient packaging and transport: Preparing the patient for transport and assisting with loading them into the ambulance.
Key Limitation: EMRs typically do not administer medications or perform advanced procedures. Their role focuses primarily on immediate stabilization and preparation for transport by higher-level providers.
Emergency Medical Technician (EMT)
EMTs possess a broader scope of practice than EMRs, incorporating more advanced BLS skills and some limited advanced life support (ALS) procedures. Their responsibilities typically encompass:
- All EMR skills: EMTs are expected to proficiently perform all the skills of an EMR.
- Advanced airway management: Utilizing advanced airway adjuncts like oral or nasal airways.
- Oxygen administration: Providing supplemental oxygen using various delivery methods.
- Automated external defibrillation (AED): Operating AEDs to deliver life-saving shocks.
- IV insertion and fluid administration: In some jurisdictions, EMTs might be authorized for intravenous (IV) insertion and fluid administration.
- Medication administration: Limited medication administration, such as oral glucose or aspirin, may be allowed, depending on local protocols.
- Advanced splinting and immobilization: Using more sophisticated splinting and immobilization techniques.
Key Differences from EMR: EMTs possess a wider range of skills, enabling them to provide more comprehensive care before the arrival of paramedics or in situations where paramedics are unavailable.
Advanced Emergency Medical Technician (AEMT)
AEMTs represent a bridge between EMTs and paramedics. They possess a more extensive scope of practice than EMTs, incorporating a greater number of ALS skills and responsibilities. This includes:
- All EMT skills: AEMTs build upon the foundation of EMT skills.
- Advanced airway management: Skills may include endotracheal intubation, advanced airway devices, and management of difficult airways.
- IV and IO access: More extensive IV and intraosseous (IO) access capabilities.
- Medication administration: A wider range of medications, administered via various routes, including IV.
- Cardiac monitoring and defibrillation: Advanced cardiac monitoring and the ability to perform synchronized cardioversion.
- 12-lead ECG interpretation: The ability to interpret 12-lead electrocardiograms (ECGs) to identify cardiac rhythms.
Key Differences from EMT: AEMTs can perform a significantly wider range of ALS procedures, enhancing their ability to provide critical care in the prehospital setting. They often serve as a crucial link between EMTs and paramedics, handling more complex cases before paramedic arrival.
Paramedic
Paramedics are the highest level of prehospital providers, possessing the most extensive scope of practice. They can perform a wide array of complex ALS interventions, including:
- All AEMT and EMT skills: Paramedics build upon the skills of lower levels, demonstrating mastery across all aspects of prehospital care.
- Advanced airway management: Advanced airway management techniques, including rapid sequence intubation (RSI).
- Advanced cardiac life support (ACLS): Comprehensive ACLS skills, including advanced cardiac arrhythmia management.
- Pharmacology: Extensive knowledge and application of a broad range of medications.
- Advanced assessment and interventions: Performing sophisticated assessments and interventions for a wide range of medical and trauma emergencies.
- Advanced monitoring capabilities: Utilizing advanced monitoring equipment, such as invasive hemodynamic monitoring.
Key Differences from AEMT: Paramedics are authorized to perform the most advanced procedures, effectively bridging the gap between prehospital and hospital care. Their skills allow them to manage extremely critical situations and provide stabilization for patients requiring immediate advanced intervention.
State Variations and Local Protocols
It's crucial to understand that the National EMS Scope of Practice Model is not a legally binding document. Individual states adapt and modify the model to align with their unique needs, resources, and legal frameworks. This results in variations in the specific procedures and medications authorized for each provider level across different states and even within different regions of the same state. Local EMS protocols further refine these state-level regulations, providing specific guidelines for EMS personnel within a particular jurisdiction. Therefore, EMS providers must always be aware of and adhere to the specific scope of practice and protocols governing their practice area.
Importance of Continuing Education and Competency
The dynamic nature of EMS necessitates continuous professional development for all levels of providers. Regular continuing education courses, advanced training programs, and ongoing competency assessments are essential to maintain skills, stay updated with the latest advancements in medical care, and ensure adherence to evolving best practices. These efforts ensure that EMS providers can consistently deliver high-quality, evidence-based care within their scope of practice.
Legal and Ethical Considerations
The National EMS Scope of Practice Model indirectly influences the legal and ethical responsibilities of EMS providers. Operating outside the defined scope of practice can lead to legal ramifications, including disciplinary action, license revocation, and even lawsuits. Ethical considerations are also crucial; providers must always act within their competency level and prioritize patient safety and well-being. Informed consent, proper documentation, and adherence to established protocols are paramount to ensuring ethical and legally sound practice.
The Future of the National EMS Scope of Practice Model
The model continues to evolve, reflecting ongoing advancements in medical technology, research, and best practices. Future iterations of the model will likely incorporate new technologies, such as telehealth integration, and address emerging challenges in prehospital care, such as the opioid crisis and mass casualty incidents. The ongoing refinement of the National EMS Scope of Practice Model ensures that EMS providers are equipped to provide the most effective and appropriate care to patients in need, reflecting the highest standards of prehospital emergency medicine.
Conclusion
The National EMS Scope of Practice Model is a cornerstone of the US EMS system. Its tiered structure provides a framework for the education, training, and practice of EMS personnel, ensuring a progressive increase in competency and responsibility. While state variations and local protocols exist, the model provides a crucial benchmark for maintaining high standards of prehospital care. Understanding this model, its implications, and its ongoing evolution is essential for all stakeholders within the EMS community. The emphasis on continuing education, adherence to protocols, and ethical practice remains paramount for ensuring the safety and well-being of patients and the continued professionalism of the EMS profession. The future of the model promises further advancements, reflecting the ongoing commitment to improving prehospital emergency care and ensuring that EMS providers remain at the forefront of delivering timely and effective interventions.
Latest Posts
Latest Posts
-
Treatment That Includes A Focus On Personal Strengths And Development
Mar 18, 2025
-
Which Is Not A Form Of Maltreatment
Mar 18, 2025
-
If An Individual Is Heterozygous For A Particular Trait
Mar 18, 2025
-
If You Add More Enzyme The Reaction Will
Mar 18, 2025
-
The Purpose Of A Hazcom Program Is To Ensure That
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about According To The National Ems Scope Of Practice Model . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
