Anaphylaxis Is Most Accurately Defined As A N
Breaking News Today
Apr 01, 2025 · 6 min read
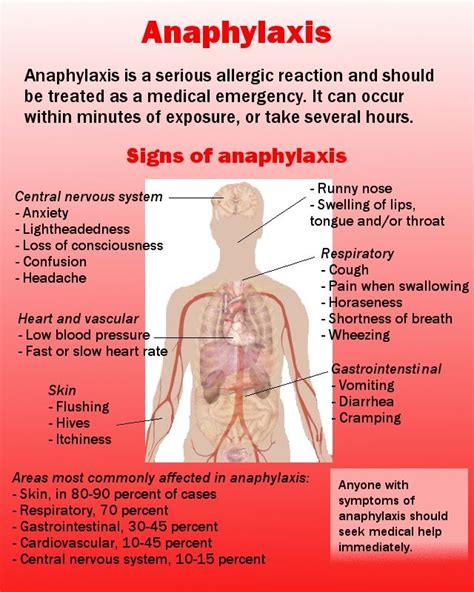
Table of Contents
Anaphylaxis: A Comprehensive Overview of This Life-Threatening Allergic Reaction
Anaphylaxis is most accurately defined as a severe, life-threatening allergic reaction that occurs rapidly and can cause death if left untreated. It's a systemic reaction, meaning it affects the entire body, and is triggered by exposure to an allergen – a substance that the body's immune system mistakenly identifies as a threat. Understanding anaphylaxis is crucial for both individuals at risk and healthcare professionals alike. This detailed article explores its causes, symptoms, diagnosis, treatment, and prevention.
Understanding the Immunology Behind Anaphylaxis
Anaphylaxis is a consequence of the body's immune system overreacting to a perceived threat. The first exposure to an allergen, such as peanuts or bee venom, sensitizes the body. This sensitization involves the production of immunoglobulin E (IgE) antibodies by specialized immune cells called plasma cells. These IgE antibodies attach themselves to mast cells and basophils, cells found throughout the body, particularly in the skin, lungs, and gastrointestinal tract.
Upon subsequent exposure to the same allergen, the allergen binds to the IgE antibodies already attached to these cells. This binding triggers a cascade of events, releasing potent inflammatory mediators, including histamine, tryptase, and leukotrienes. These mediators cause the characteristic symptoms of anaphylaxis. The severity of the reaction depends on several factors, including the dose of the allergen, the route of exposure (e.g., ingestion, injection), and the individual's sensitivity.
The Role of Histamine and Other Mediators
Histamine is a primary mediator responsible for many of the early symptoms of anaphylaxis. It causes vasodilation (widening of blood vessels), increased capillary permeability (leakiness of blood vessels), bronchoconstriction (narrowing of the airways), and increased mucus secretion. Tryptase, another mediator released from mast cells, is a more specific marker for anaphylaxis and can be measured in blood tests to help confirm a diagnosis. Leukotrienes contribute to prolonged bronchoconstriction and inflammation. This complex interplay of mediators explains the wide range of symptoms associated with anaphylaxis.
Common Triggers of Anaphylaxis
A wide variety of substances can trigger anaphylactic reactions. Identifying these triggers is crucial for prevention and management. Some of the most common include:
- Foods: Peanuts, tree nuts (walnuts, cashews, pecans, etc.), milk, eggs, soy, wheat, fish, and shellfish are frequent culprits. Even trace amounts can trigger a reaction in highly sensitive individuals.
- Insect stings: Bee stings, wasp stings, hornet stings, and ant stings are common causes, especially in individuals with venom allergies.
- Medications: Penicillin and other beta-lactam antibiotics, aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), and contrast dyes used in medical imaging are some examples.
- Latex: Exposure to latex products, such as gloves and balloons, can cause anaphylaxis in susceptible individuals.
- Other potential triggers: Exercise, certain chemicals (e.g., venom from certain species of jellyfish), and even certain types of physical stimuli (e.g. cold exposure, vibratory stimuli) can, less frequently, initiate anaphylactic events.
Recognizing the Signs and Symptoms of Anaphylaxis
Anaphylaxis symptoms can manifest rapidly, typically within minutes to hours after exposure to the allergen, though occasionally delayed reactions occur. The symptoms are diverse and can affect multiple organ systems, making early recognition crucial. Key symptoms include:
- Skin and Mucous Membranes: Hives (urticaria), itching, flushing, swelling (angioedema), especially around the face, lips, and tongue.
- Respiratory System: Wheezing, shortness of breath, difficulty breathing, cough, feeling of tightness in the chest, hoarseness.
- Cardiovascular System: Rapid pulse, drop in blood pressure (hypotension), dizziness, lightheadedness, fainting (syncope).
- Gastrointestinal System: Nausea, vomiting, abdominal cramps, diarrhea.
- Neurological System: Anxiety, confusion, loss of consciousness.
Differentiating Anaphylaxis from Other Allergic Reactions
It’s essential to differentiate anaphylaxis from other, less severe allergic reactions. While symptoms like hives and itching can occur in both, anaphylaxis involves a combination of symptoms affecting multiple organ systems and a rapid onset. The presence of respiratory compromise (wheezing, shortness of breath) or cardiovascular collapse (hypotension, fainting) is particularly indicative of anaphylaxis.
Diagnosing Anaphylaxis
Diagnosing anaphylaxis often relies on the clinical presentation – the patient's symptoms and history. A detailed medical history, including a careful assessment of potential triggers and the timeline of symptom development, is paramount. While there isn't one definitive diagnostic test for anaphylaxis, several investigations can support the diagnosis:
- Tryptase levels: Measuring tryptase levels in the blood can be helpful, especially if the test is performed within a few hours of the reaction. Elevated levels suggest mast cell activation.
- Skin prick tests or patch tests: These tests can identify specific allergens that may be responsible for the reaction.
- Allergy blood tests (serum-specific IgE): These tests measure the level of IgE antibodies specific to different allergens.
Treatment of Anaphylaxis: Prompt Action is Crucial
Treatment of anaphylaxis is a medical emergency requiring immediate intervention. The primary treatment is epinephrine (adrenaline), administered via intramuscular injection using an auto-injector (like an EpiPen or Auvi-Q). Epinephrine acts to reverse many of the effects of the inflammatory mediators, constricting blood vessels, relaxing airways, and improving cardiac function.
Steps in Anaphylactic Treatment
- Administer Epinephrine: This is the cornerstone of anaphylaxis treatment. A second dose may be necessary if symptoms don't improve or worsen.
- Airway Management: Ensure a patent airway, potentially using supplemental oxygen or advanced airway techniques if necessary.
- Fluid Resuscitation: Intravenous fluids may be administered to treat hypotension.
- Monitoring: Close monitoring of vital signs (blood pressure, heart rate, respiratory rate, oxygen saturation) is essential.
- Further Treatment: Additional medications such as antihistamines (e.g., diphenhydramine), corticosteroids (e.g., methylprednisolone), and beta-agonists (e.g., albuterol) may be given to alleviate symptoms and prevent recurrence.
Preventing Anaphylaxis: Proactive Measures are Key
Prevention is the most effective strategy in managing anaphylaxis. This involves identifying and avoiding triggers, carrying an emergency epinephrine auto-injector, and educating individuals and their families about the condition.
Key Preventive Strategies
- Allergen Avoidance: Careful avoidance of known allergens is crucial. This involves reading food labels carefully, wearing medical alert bracelets, and avoiding exposure to insect stings.
- Epinephrine Auto-injector Training: Individuals at risk should carry and be trained on the use of an epinephrine auto-injector. Regularly check the expiry date and replace as needed.
- Emergency Action Plan: Develop and practice an emergency action plan with family and friends. This should include details of the individual’s allergies, the steps to take in case of an anaphylactic reaction, and emergency contact information.
- Medical Alert Identification: Wearing a medical alert bracelet or necklace clearly identifying allergies is essential.
- Regular Follow-Up: Regular check-ups with an allergist are recommended to monitor for changes in sensitivity and to adjust treatment plans as needed.
Living with Anaphylaxis: Managing the Condition Effectively
Living with the risk of anaphylaxis requires a proactive and informed approach. Individuals and their families need to understand the condition thoroughly, implement preventative measures consistently, and be prepared for emergencies. Regular consultations with an allergist, careful adherence to medication regimens, and maintaining a well-defined emergency action plan are vital components of effective management.
Empowering Individuals and Families
Effective management involves empowering individuals and their families to understand the condition's intricacies. This includes knowledge of triggers, symptom recognition, appropriate treatment, and preventive strategies. Open communication with healthcare professionals, schools (if applicable), and workplaces is essential to ensure a safe environment.
Conclusion: A Multifaceted Approach to Anaphylaxis
Anaphylaxis is a potentially fatal allergic reaction requiring prompt recognition and treatment. Understanding its underlying immunology, common triggers, symptoms, diagnosis, and treatment is paramount for healthcare professionals and individuals at risk. A multifaceted approach, combining allergen avoidance, epinephrine auto-injector use, emergency preparedness, and regular medical follow-up, is essential for effectively managing and preventing this life-threatening condition. Early intervention and a proactive approach to prevention are key to minimizing the risk and ensuring the safety and well-being of those affected.
Latest Posts
Latest Posts
-
According To Texass Attorney Why Should The Flag Be Protected
Apr 02, 2025
-
When Assessing A Patient With A Medical Complaint
Apr 02, 2025
-
Schizoid Personality Disorder Differs From Paranoid Personality Disorder In That
Apr 02, 2025
-
Amoeba Sisters Video Recap Answer Key Cell Transport
Apr 02, 2025
-
What Does Extension Of A Point Refer To
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Anaphylaxis Is Most Accurately Defined As A N . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
