Anaphylaxis Is Most Accurately Defined As An
Breaking News Today
Mar 27, 2025 · 6 min read
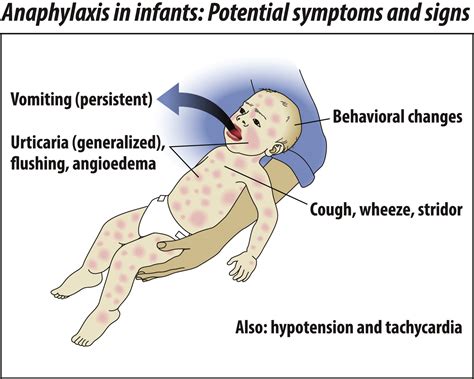
Table of Contents
Anaphylaxis: A Comprehensive Overview
Anaphylaxis is most accurately defined as a severe, life-threatening, systemic allergic reaction. It's characterized by a rapid onset of symptoms and can involve multiple organ systems. Understanding its precise definition is crucial, as it dictates the urgency of treatment and the potential for fatal consequences. This article will delve into the intricacies of anaphylaxis, exploring its causes, symptoms, diagnosis, treatment, and preventative measures.
What Causes Anaphylaxis?
Anaphylaxis is triggered by an allergic reaction to a substance, known as an allergen. This allergen interacts with the body's immune system, specifically immunoglobulin E (IgE) antibodies, leading to a cascade of events that cause a widespread inflammatory response. Common triggers include:
Common Allergens:
- Foods: Peanuts, tree nuts (almonds, walnuts, cashews), milk, eggs, soy, wheat, fish, and shellfish are frequent culprits. Even trace amounts can trigger a reaction in highly sensitive individuals.
- Insect stings: Bee, wasp, hornet, and ant stings are notorious for causing anaphylaxis, especially in individuals with pre-existing allergies.
- Medications: Penicillin, aspirin, and other nonsteroidal anti-inflammatory drugs (NSAIDs) are among the medications that can induce anaphylaxis. Contrast dyes used in medical imaging are also potential triggers.
- Latex: Exposure to latex products, such as gloves and balloons, can cause severe allergic reactions in sensitive individuals.
- Other potential triggers: Exercise, certain chemicals (e.g., in cosmetics or cleaning products), and even certain types of physical stimuli (e.g., cold temperatures) can, in rare cases, trigger anaphylactic reactions.
The Immunological Mechanism:
The underlying mechanism involves the interaction between the allergen and pre-formed IgE antibodies attached to mast cells and basophils. Upon exposure to the allergen, these cells release various mediators, including histamine, tryptase, and leukotrienes. These mediators are responsible for the characteristic symptoms of anaphylaxis. The release of these mediators causes widespread vasodilation (widening of blood vessels), bronchoconstriction (narrowing of airways), and increased vascular permeability (leakiness of blood vessels).
Recognizing the Symptoms of Anaphylaxis:
Anaphylaxis symptoms can vary in severity and presentation, depending on the individual and the allergen involved. However, some common signs and symptoms include:
Common Signs and Symptoms:
- Skin manifestations: Hives (urticaria), itching, flushing, swelling (angioedema), especially around the face, lips, tongue, and throat.
- Respiratory symptoms: Wheezing, shortness of breath, cough, difficulty breathing, and feeling of tightness in the chest.
- Cardiovascular symptoms: Rapid or weak pulse, low blood pressure (hypotension), dizziness, fainting, and even cardiac arrest.
- Gastrointestinal symptoms: Nausea, vomiting, abdominal cramps, and diarrhea.
- Neurological symptoms: Dizziness, confusion, loss of consciousness, and even seizures.
Understanding the Severity:
The severity of anaphylaxis is highly variable. Some individuals may experience only mild symptoms, such as hives and itching, while others may experience a life-threatening cascade of events leading to respiratory compromise or cardiovascular collapse. The speed of symptom onset is a critical factor; rapid progression of symptoms strongly suggests anaphylaxis.
Diagnosing Anaphylaxis:
Diagnosing anaphylaxis can be challenging, particularly when symptoms are not immediately apparent or are atypical. The diagnosis is primarily based on clinical presentation, meaning the doctor relies heavily on the patient's symptoms and history.
Diagnostic Criteria:
While there isn't a single definitive test for anaphylaxis, the diagnosis is typically made using criteria that consider the patient's history, physical examination, and response to treatment. These include:
- Acute onset of symptoms: Rapid development of symptoms, usually within minutes to hours of exposure to the allergen.
- Involvement of multiple organ systems: Symptoms affecting at least two organ systems (e.g., skin and respiratory).
- Hypotension or other cardiovascular compromise: Low blood pressure, rapid or weak pulse, or signs of shock.
- Response to treatment: Dramatic improvement of symptoms after administering epinephrine.
Testing for Allergies:
Although not directly diagnosing anaphylaxis, allergy testing, such as skin prick tests or blood tests (RAST), can help identify specific allergens that might trigger future reactions. This information is vital for preventative strategies and developing an individual's allergy management plan.
Treating Anaphylaxis:
Treatment for anaphylaxis is a medical emergency. Immediate administration of epinephrine (adrenaline) is crucial. This medication counteracts the effects of the allergic mediators, improving blood pressure, reducing airway constriction, and relieving symptoms.
Epinephrine: The First-Line Treatment:
Epinephrine should be administered intramuscularly (into the thigh) using an auto-injector (EpiPen, Auvi-Q). This is generally the first and most important step in managing anaphylaxis. Further medical interventions may be necessary depending on the severity of the reaction.
Other Treatment Modalities:
In addition to epinephrine, other treatments may be necessary to support vital functions. These might include:
- Oxygen supplementation: To improve oxygen levels in the blood.
- Intravenous fluids: To maintain blood pressure.
- Bronchodilators: To relax the airways and improve breathing.
- Antihistamines: To reduce the effects of histamine.
- Corticosteroids: To reduce inflammation.
Preventing Anaphylaxis:
Preventing anaphylaxis involves understanding your triggers and taking appropriate precautions. This is a critical aspect of managing allergies and reducing the risk of future reactions.
Strategies for Prevention:
- Allergen avoidance: This is the cornerstone of prevention. Carefully reading food labels, avoiding known allergens, and taking precautions against insect stings are essential.
- Medical alert bracelets or necklaces: Wearing medical identification clearly stating allergies can alert medical personnel in case of an emergency.
- Emergency action plan: Developing a personalized plan that details steps to take during an anaphylactic reaction can save valuable time during an emergency.
- Carrying an epinephrine auto-injector: Always have an epinephrine auto-injector readily available, ensuring it is not expired and you know how to use it.
- Regular consultations with an allergist: Staying up-to-date on allergy management through regular consultations with a specialist can ensure your safety and preparedness.
Anaphylaxis in Children:
Children are particularly vulnerable to anaphylaxis due to their developing immune systems and often limited ability to communicate symptoms. Parents and caregivers need to be vigilant and equipped with the knowledge and tools to recognize and respond effectively to anaphylactic reactions in children.
Specific Considerations for Children:
- Early recognition of symptoms: It’s crucial for parents to recognize the signs and symptoms of anaphylaxis in children, which may be different from those in adults.
- Proper epinephrine administration: Parents and caregivers should receive thorough training on administering epinephrine via an auto-injector.
- School emergency plans: Working with schools to develop an emergency plan for managing anaphylaxis is important to ensure timely treatment in case of a reaction.
The Future of Anaphylaxis Management:
Research continues to advance our understanding of anaphylaxis and improve its management. This includes ongoing research into new treatments, diagnostic tools, and preventative strategies.
Areas of Ongoing Research:
- Developing more effective treatments: Researchers are continually searching for improved therapies to better manage anaphylactic reactions.
- Improving diagnostic methods: More accurate and rapid diagnostic methods are being developed to facilitate early intervention.
- Exploring novel preventative strategies: Research is ongoing to explore innovative methods for preventing anaphylaxis, including potential therapies to desensitize individuals to allergens.
Conclusion:
Anaphylaxis is a severe, life-threatening condition requiring immediate medical attention. Understanding its causes, symptoms, diagnosis, treatment, and prevention is vital for both individuals with allergies and healthcare professionals. Early recognition and prompt treatment with epinephrine are crucial for minimizing the risk of severe complications and ensuring patient safety. With increased awareness, effective management strategies, and ongoing research, the outlook for individuals at risk of anaphylaxis continues to improve. Always consult a healthcare professional for accurate diagnosis, treatment, and personalized management plans.
Latest Posts
Latest Posts
-
Most Surface Ocean Waves Are Caused By
Mar 30, 2025
-
A Large Portion Of Inspector Communication Involves
Mar 30, 2025
-
Which Of The Following Best Describes A Like Plan Change
Mar 30, 2025
-
Tus Disquetes Encima De La Computadora
Mar 30, 2025
-
Suggested Initial Dose Of Epinephrine Nrp 8th Edition
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about Anaphylaxis Is Most Accurately Defined As An . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
