Bleeding From Soft Tissue Injuries To The Face
Breaking News Today
Mar 20, 2025 · 6 min read
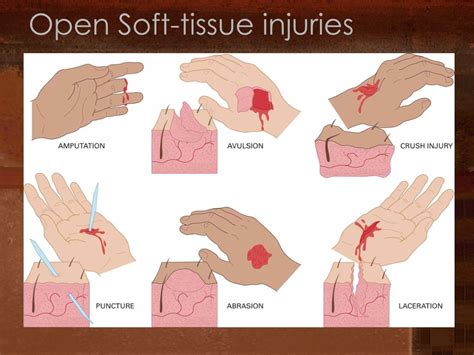
Table of Contents
- Bleeding From Soft Tissue Injuries To The Face
- Table of Contents
- Bleeding from Soft Tissue Injuries to the Face: A Comprehensive Guide
- Causes of Facial Soft Tissue Bleeding
- Traumatic Injuries:
- Non-Traumatic Causes:
- Assessment of Facial Soft Tissue Bleeding
- Initial Assessment:
- Detailed Examination:
- Management of Facial Soft Tissue Bleeding
- First Aid Measures:
- Medical Interventions:
- Prevention of Facial Soft Tissue Injuries
- Safety Measures:
- Long-Term Care and Complications
- Wound Care:
- Potential Complications:
- Conclusion
- Latest Posts
- Latest Posts
- Related Post
Bleeding from Soft Tissue Injuries to the Face: A Comprehensive Guide
Facial injuries, particularly those involving soft tissue, can result in significant bleeding. Understanding the causes, assessment, management, and prevention of such injuries is crucial for both healthcare professionals and the general public. This comprehensive guide delves into the intricacies of facial soft tissue bleeding, providing detailed information to enhance knowledge and improve response strategies.
Causes of Facial Soft Tissue Bleeding
Facial soft tissue injuries encompass a wide range of traumas, each capable of causing bleeding varying in severity. Understanding the causative factors is paramount for effective management.
Traumatic Injuries:
-
Blunt force trauma: This is a common cause, ranging from minor bumps and bruises to severe lacerations and fractures. Impacts from falls, assaults, sports accidents, and motor vehicle collisions can all inflict significant damage to the face, leading to bleeding from broken blood vessels. The severity depends on the force of impact and the location of the injury.
-
Penetrating injuries: These injuries involve objects piercing the skin and underlying tissues, such as stab wounds, gunshot wounds, or impalement injuries. Penetrating injuries often cause profuse bleeding due to the direct damage to blood vessels and the potential involvement of major arteries.
-
Lacerations: Cuts and tears in the skin and underlying tissues are categorized as lacerations. Their depth and location determine the extent of bleeding. Deep lacerations, especially those involving facial muscles and nerves, can bleed heavily.
-
Avulsions: These are injuries where a portion of tissue is torn away from the body. Avulsions are often associated with significant bleeding and require immediate medical attention. Facial avulsions are particularly concerning due to the potential for cosmetic and functional impairment.
Non-Traumatic Causes:
While less common, certain non-traumatic conditions can also lead to facial bleeding:
-
Medical conditions: Hemophilia and other bleeding disorders can result in prolonged and excessive bleeding from even minor facial injuries. Similarly, certain medications, such as anticoagulants (blood thinners), can increase the risk of bleeding.
-
Infections: Severe facial infections can cause tissue breakdown and bleeding. Conditions like cellulitis or necrotizing fasciitis can lead to extensive soft tissue damage and haemorrhage.
-
Spontaneous bleeding: Rarely, spontaneous bleeding can occur in the face due to vascular malformations or other underlying medical conditions.
Assessment of Facial Soft Tissue Bleeding
Effective management begins with a thorough assessment of the injury. This involves a systematic evaluation to determine the severity of the bleeding and the underlying cause.
Initial Assessment:
-
Control bleeding: The initial priority is to control the bleeding. Apply direct pressure to the wound using a clean cloth. Elevation of the injured area can also help reduce bleeding.
-
Assess airway, breathing, and circulation (ABCs): Ensure the patient’s airway is clear, breathing is adequate, and circulation is stable. Severe facial injuries can compromise these vital functions.
-
Identify the type and location of the injury: Determine if the bleeding is from a laceration, avulsion, or other injury. Note the precise location to assist in assessing potential complications.
-
Evaluate the extent of bleeding: Assess the amount of blood loss. Significant bleeding might indicate the involvement of major blood vessels or arteries.
-
Look for signs of shock: Monitor vital signs (heart rate, blood pressure, respiratory rate) for signs of shock, such as pale skin, rapid pulse, and low blood pressure.
Detailed Examination:
Once the immediate threat is addressed, a more detailed examination is necessary:
-
Visual inspection: Carefully inspect the wound to determine its depth, length, and involvement of underlying structures like muscles, nerves, or bones.
-
Palpation: Gently palpate the area to identify any fractures, foreign bodies, or significant tissue damage.
-
Neurological assessment: Assess facial nerve function by checking for any numbness, tingling, or weakness in the face.
-
Check for underlying injuries: Facial injuries can be associated with other injuries, such as skull fractures, brain injuries, or injuries to the eyes or teeth.
Management of Facial Soft Tissue Bleeding
Management strategies depend on the severity of the bleeding and the nature of the injury. Simple injuries may require only basic first aid, while severe injuries necessitate immediate medical intervention.
First Aid Measures:
-
Direct pressure: Applying firm, direct pressure to the wound using a clean cloth is the first line of defense against bleeding. Maintain pressure for at least 10-15 minutes.
-
Elevation: Elevating the injured area can help reduce swelling and bleeding.
-
Cold compress: A cold compress can help constrict blood vessels and reduce swelling.
-
Clean the wound: Once bleeding is controlled, gently clean the wound with sterile saline or clean water. Avoid using harsh chemicals or abrasive materials.
Medical Interventions:
-
Wound closure: Lacerations may require sutures (stitches) or surgical closure to stop bleeding and promote healing. The choice of technique depends on the depth, location, and extent of the laceration.
-
Surgical repair: Avulsions and complex injuries often require surgical repair to restore tissue integrity and minimize scarring. This may involve tissue grafts or flaps.
-
Blood transfusion: In cases of significant blood loss, a blood transfusion may be necessary to restore blood volume and maintain vital functions.
-
Antibiotics: Antibiotics may be prescribed to prevent infection, particularly in deep wounds or those with a high risk of contamination.
-
Pain management: Analgesics (pain relievers) may be necessary to manage pain and discomfort.
-
Tetanus prophylaxis: Ensure the patient has received a tetanus booster within the past 10 years.
Prevention of Facial Soft Tissue Injuries
Prevention is always preferable to treatment. Many facial injuries are preventable by taking appropriate precautions.
Safety Measures:
-
Wear protective gear: Wear helmets, face shields, and other protective gear during activities that carry a risk of facial injury, such as contact sports, cycling, and motorcycling.
-
Secure loose objects: Secure any loose objects in your home or workplace that could cause facial injuries.
-
Practice safe driving: Follow traffic laws and drive defensively to reduce the risk of motor vehicle accidents.
-
Avoid alcohol and drug use: Alcohol and drug use impair judgment and coordination, increasing the risk of accidents.
Long-Term Care and Complications
Following a facial soft tissue injury, proper aftercare is crucial to minimize scarring and complications.
Wound Care:
-
Keep the wound clean and dry: Regularly clean the wound as instructed by your healthcare provider. Avoid touching or picking at the wound.
-
Change dressings: Change dressings regularly to prevent infection.
-
Monitor for signs of infection: Monitor the wound for signs of infection, such as redness, swelling, pain, pus, or fever.
Potential Complications:
-
Scarring: Scarring is a common complication of facial injuries. The extent of scarring depends on the severity of the injury and the quality of wound care.
-
Infection: Infection can occur if the wound is not properly cleaned and cared for.
-
Facial nerve damage: Damage to facial nerves can lead to facial paralysis or weakness.
-
Cosmetic deformity: Severe injuries can result in cosmetic deformities that may require reconstructive surgery.
Conclusion
Bleeding from soft tissue injuries to the face can range from minor to life-threatening. A thorough understanding of the causes, assessment, management, and prevention of these injuries is crucial for effective care. Early intervention, proper first aid, and timely medical attention can significantly improve outcomes and minimize long-term complications. Remember, prevention is key; adopting appropriate safety measures can greatly reduce the risk of facial injuries. Always seek professional medical advice for any significant facial injury. This information is for educational purposes only and does not substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment of any medical condition.
Latest Posts
Latest Posts
-
Texas Jurisprudence Exam Questions And Answers Pdf
Mar 21, 2025
-
Struck By Injuries Are Produced By Forcible Contact
Mar 21, 2025
-
Bladder Retraining Following Removal Of An Indwelling Catheter Begins With
Mar 21, 2025
-
Identify The Defining Characteristics Of An Organization
Mar 21, 2025
-
This Seals Up Gaps In A Piece Of Dna
Mar 21, 2025
Related Post
Thank you for visiting our website which covers about Bleeding From Soft Tissue Injuries To The Face . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
