Describe Neural And Chemical Control Of Ventilation During Exercise.
Breaking News Today
Mar 17, 2025 · 7 min read
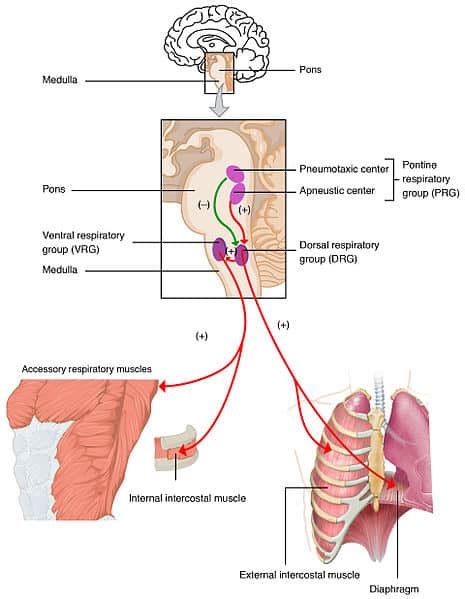
Table of Contents
Neural and Chemical Control of Ventilation During Exercise
Exercise presents a significant physiological challenge, demanding a dramatic increase in oxygen uptake and carbon dioxide removal. This heightened metabolic demand necessitates precise and coordinated control of ventilation – the process of breathing – to ensure adequate gas exchange. This control is achieved through a complex interplay of neural and chemical mechanisms, working in concert to match ventilation to the body's metabolic needs. Understanding this intricate control system is crucial to comprehending both the physiological adaptations to exercise and the pathophysiology of exercise-related respiratory disorders.
Neural Control: Setting the Stage for Respiratory Adaptation
The neural control of ventilation during exercise originates primarily in the brainstem, specifically within the medulla oblongata and pons. These regions house respiratory centers containing groups of neurons responsible for generating the rhythmic pattern of breathing. However, the brainstem respiratory centers don't act in isolation; they receive a constant barrage of afferent input from various peripheral and central sources, influencing the respiratory output and adjusting ventilation in response to exercise.
Peripheral Chemoreceptors: Sensing Changes in Blood Gases
Peripheral chemoreceptors, located in the carotid bodies and aortic bodies, play a crucial role in detecting changes in arterial blood gas levels. These chemoreceptors are exquisitely sensitive to decreases in partial pressure of oxygen (PaO2) and increases in partial pressure of carbon dioxide (PaCO2), as well as increases in hydrogen ion concentration (pH – reflecting acidosis).
During exercise, the increased metabolic rate leads to a rise in PaCO2 and a fall in pH (due to lactic acid production). These changes stimulate the peripheral chemoreceptors, sending increased afferent signals to the brainstem respiratory centers. This results in an immediate increase in ventilation, helping to eliminate the excess CO2 and restore acid-base balance. While the effect of PaO2 on ventilation is typically less significant at rest, its influence becomes more prominent during intense exercise, especially at high altitudes where PaO2 is inherently lower.
Central Chemoreceptors: Monitoring Brain CO2 Levels
Central chemoreceptors, located in the medulla oblongata, are primarily sensitive to changes in the pH of the cerebrospinal fluid (CSF). Although they don't directly detect PaCO2, the CO2 readily crosses the blood-brain barrier and reacts with water in the CSF to form carbonic acid (H2CO3), which dissociates into hydrogen ions (H+) and bicarbonate ions (HCO3-). The resulting increase in H+ concentration in the CSF stimulates the central chemoreceptors.
During exercise, the rise in PaCO2 leads to a corresponding increase in CSF H+, stimulating the central chemoreceptors and contributing to the overall increase in ventilation. The central chemoreceptors play a more sustained role in ventilatory control during exercise compared to the peripheral chemoreceptors, maintaining the elevated ventilation even as the acute changes in PaCO2 and pH are partially buffered.
Mechanoreceptors: Providing Sensory Feedback
Mechanoreceptors located throughout the body provide afferent feedback to the brainstem respiratory centers based on mechanical stimuli. These include:
-
Lung receptors: Stretch receptors in the lung parenchyma respond to lung inflation, contributing to the Hering-Breuer reflex that prevents overinflation. During exercise, this reflex may play a minor role in adjusting respiratory rate. Irritant receptors in the airways respond to noxious stimuli (e.g., dust, irritants), initiating cough and bronchoconstriction. These responses are less directly involved in the overall control of ventilation during exercise.
-
Muscle receptors: Muscle spindles and Golgi tendon organs in exercising muscles sense changes in muscle length and tension. These receptors send signals to the brainstem, contributing to the anticipatory increase in ventilation that occurs before the onset of exercise. This anticipatory response is partly mediated by neural pathways involving the motor cortex and brainstem. Additionally, metaboreceptors within muscles detect metabolic byproducts like lactate and potassium ions, contributing to the ventilatory response.
-
Joint receptors: Joint receptors provide information about limb movement and position. Their input contributes to the overall increase in ventilation during exercise, although their precise role is still under investigation.
Chemical Control: The Metabolic Influence on Breathing
The chemical control of ventilation during exercise is intimately linked to the metabolic demands of the exercising muscles. The increased metabolic rate leads to several changes in the body's internal environment that directly or indirectly influence breathing:
Carbon Dioxide (CO2): The Primary Stimulus
As mentioned earlier, the rise in PaCO2 during exercise is a potent stimulus for increased ventilation. This increase in CO2 is a direct consequence of the enhanced metabolic rate and the increased production of CO2 as a byproduct of cellular respiration. The resulting increase in PaCO2 stimulates both peripheral and central chemoreceptors, leading to a rapid and substantial increase in ventilation.
Hydrogen Ions (H+): Acid-Base Balance and Ventilation
The accumulation of lactic acid during intense exercise leads to a decrease in blood pH (acidosis). This acidosis stimulates both peripheral and central chemoreceptors, contributing to the increase in ventilation. The increased ventilation helps to eliminate CO2, which indirectly reduces H+ concentration by shifting the carbonic acid equilibrium. The body's buffering systems also play a vital role in mitigating the effects of acidosis.
Oxygen (O2): A Modulatory Role
While CO2 and H+ are the primary chemical drivers of ventilation during exercise, oxygen also plays a role, particularly during intense or prolonged exercise. A decrease in PaO2 (hypoxia), either due to high-intensity exercise or altitude, stimulates the peripheral chemoreceptors, increasing ventilation. However, the hypoxic drive is usually less significant than the hypercapnic (high CO2) and acidotic drives. It becomes more crucial under conditions where oxygen supply is compromised, such as at high altitude.
Other Chemical Factors
Several other chemical factors may play a more subtle role in modulating ventilation during exercise:
- Potassium ions (K+): Increased K+ concentration in the blood, associated with muscle activity, can stimulate chemoreceptors and contribute to the increase in ventilation.
- Adrenaline and noradrenaline: These hormones, released during exercise, can directly stimulate the respiratory centers and contribute to increased ventilation.
- Lactate: Although primarily involved in acid-base balance, lactate itself may have direct effects on ventilation, independent of its role in reducing pH.
Integration of Neural and Chemical Control During Exercise
The neural and chemical control mechanisms of ventilation during exercise don't function in isolation; they are intricately integrated to provide a finely tuned response to the body's metabolic demands. The anticipatory increase in ventilation that precedes exercise is primarily neurally mediated, involving input from higher brain centers and muscle afferents. However, this anticipatory response is then further amplified and fine-tuned by the chemical stimuli arising from the increased metabolic rate.
The interplay between these systems ensures that ventilation is precisely matched to the oxygen demand and carbon dioxide production of the exercising muscles. During moderate exercise, the increase in ventilation is primarily driven by the chemical stimuli, with neural input playing a supporting role. However, during intense exercise, the neural input becomes more prominent, potentially contributing to a more forceful and rapid increase in ventilation.
Individual Variability and Training Effects
The response of the ventilatory system to exercise is not uniform across individuals. Factors such as age, fitness level, and underlying health conditions can influence the magnitude and timing of the ventilatory response. For example, well-trained athletes exhibit a lower ventilatory response to a given workload compared to untrained individuals, reflecting adaptations in both respiratory muscle function and central respiratory control.
Training adaptations may include:
- Increased respiratory muscle strength and endurance: Allowing for more efficient breathing.
- Enhanced efficiency of gas exchange: Reducing the need for excessive ventilation.
- Improved central respiratory control: Leading to a more appropriate and economical ventilatory response.
Clinical Implications
Disruptions in the neural and chemical control of ventilation can have significant clinical implications. Conditions such as chronic obstructive pulmonary disease (COPD), asthma, and neuromuscular disorders can impair the ability of the respiratory system to meet the demands of exercise. Understanding the underlying mechanisms of ventilatory control is essential for developing effective therapeutic strategies for these conditions. Furthermore, this knowledge informs our understanding of exercise-induced asthma and other exercise-related respiratory problems.
Conclusion
The neural and chemical control of ventilation during exercise is a complex and highly integrated system, designed to precisely match ventilation to the body's metabolic needs. The interplay between peripheral and central chemoreceptors, mechanoreceptors, and the influence of various chemical factors ensures that sufficient oxygen is delivered and carbon dioxide is removed, maintaining homeostasis during even the most strenuous physical activity. Understanding this intricate control system provides crucial insights into both the physiological adaptations to exercise and the pathophysiology of respiratory disorders, informing both training strategies and clinical management. Further research continues to refine our understanding of this essential physiological process.
Latest Posts
Latest Posts
-
If An Individual Is Heterozygous For A Particular Trait
Mar 18, 2025
-
If You Add More Enzyme The Reaction Will
Mar 18, 2025
-
The Purpose Of A Hazcom Program Is To Ensure That
Mar 18, 2025
-
Describe The Continuous Nature Of The Physical Fitness Concept
Mar 18, 2025
-
High Levels Of Cholesterol Can First Lead Directly To
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Describe Neural And Chemical Control Of Ventilation During Exercise. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
