Endogenous Infectious Agents Arise From Microbes That Are
Breaking News Today
Mar 22, 2025 · 6 min read
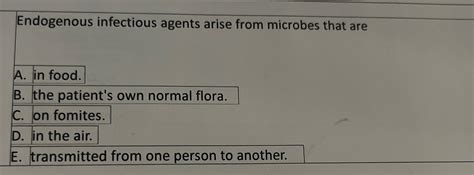
Table of Contents
- Endogenous Infectious Agents Arise From Microbes That Are
- Table of Contents
- Endogenous Infectious Agents: Arise from Microbes That Are Already Present Within the Body
- The Normal Microbiota: A Double-Edged Sword
- Common Endogenous Infectious Agents and Their Mechanisms
- 1. Bacteria:
- 2. Fungi:
- 3. Viruses:
- Diagnosing Endogenous Infections
- Treatment and Prevention of Endogenous Infections
- Conclusion: The Complex Interplay of Host and Microbe
- Latest Posts
- Latest Posts
- Related Post
Endogenous Infectious Agents: Arise from Microbes That Are Already Present Within the Body
Endogenous infectious agents represent a unique challenge in the field of infectious disease. Unlike exogenous infections, which originate from external sources, endogenous infections arise from microbes that are already present within the body, often part of the normal microbiota. These microbes, typically harmless commensals, can become pathogenic under specific circumstances, leading to a range of diseases. Understanding the mechanisms behind this transition from commensal to pathogen is crucial for effective diagnosis, treatment, and prevention.
The Normal Microbiota: A Double-Edged Sword
The human body is home to a vast and diverse community of microorganisms, collectively known as the microbiota or microbiome. This microbiota resides on the skin, in the gut, and in other mucosal surfaces. The majority of these microorganisms are beneficial, playing vital roles in:
- Nutrient metabolism: Microbes in the gut, for instance, aid in the digestion and absorption of nutrients.
- Immune system development: The microbiota helps train the immune system, distinguishing between harmless and harmful substances.
- Protection against pathogens: Beneficial microbes compete with pathogens for resources, preventing colonization and infection.
However, this same microbiota can also be a source of endogenous infection. Several factors can disrupt the delicate balance within the microbiota, leading to an opportunistic infection:
- Immune deficiency: Individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or undergoing immunosuppressive therapy, are more susceptible to endogenous infections. Their compromised immune response allows normally harmless microbes to proliferate and cause disease.
- Antibiotic use: Broad-spectrum antibiotics can disrupt the normal microbiota, leading to dysbiosis – an imbalance in the microbial community. This can create an opportunity for opportunistic pathogens to establish themselves.
- Changes in the microbiome: Various factors, including diet, stress, and environmental exposure, can alter the composition of the microbiome. This shift can lead to the overgrowth of potentially pathogenic microbes.
- Trauma or surgery: Surgical procedures or injuries can introduce microbes from the normal microbiota into normally sterile sites, leading to infection.
- Underlying diseases: Conditions like diabetes and cystic fibrosis can create an environment that favors the growth of specific pathogens.
Common Endogenous Infectious Agents and Their Mechanisms
Several types of microbes from the normal microbiota can cause endogenous infections. These include:
1. Bacteria:
- Staphylococcus aureus: A common inhabitant of the skin and nasal passages, S. aureus can cause a wide range of infections, from skin boils to life-threatening sepsis, particularly in individuals with compromised immune systems. Its virulence factors, including toxins and enzymes, contribute to its pathogenicity. The development of antibiotic resistance is a major concern.
- Streptococcus pneumoniae: Found in the upper respiratory tract, S. pneumoniae is a leading cause of pneumonia, meningitis, and otitis media. Its polysaccharide capsule helps it evade the immune system, promoting infection. Vaccination is crucial in preventing these serious infections.
- Escherichia coli: A normal inhabitant of the gut, certain strains of E. coli can cause urinary tract infections (UTIs), bloodstream infections, and other serious illnesses, especially in individuals with compromised immune systems or those with underlying conditions that disrupt the normal gut flora. Its ability to adhere to epithelial cells and produce toxins contributes to its pathogenicity.
- Pseudomonas aeruginosa: While often a commensal inhabitant of the skin and gut, P. aeruginosa is a particularly opportunistic pathogen frequently found in hospital settings. It can cause infections in the lungs (pneumonia), urinary tract (UTIs), bloodstream, and wounds. Its high antibiotic resistance is a major public health challenge.
- Enterococcus species: These bacteria are part of the normal gut flora. However, they can become pathogenic, leading to urinary tract infections (UTIs), bloodstream infections (bacteremia), and endocarditis (infection of the heart valves). Their propensity for developing antibiotic resistance makes them a serious threat.
2. Fungi:
- Candida albicans: A yeast that commonly resides in the gastrointestinal tract and other mucosal surfaces. It can cause candidiasis (thrush), a fungal infection affecting the mouth, vagina, and other areas. Immune deficiency and antibiotic use are risk factors.
- Aspergillus species: These molds are ubiquitous in the environment. In immunocompromised individuals, they can cause aspergillosis, a potentially fatal fungal infection affecting the lungs and other organs.
3. Viruses:
While viruses typically enter the body from external sources, certain viruses can remain latent within the body for extended periods and reactivate later, causing endogenous infections. This is often seen with:
- Herpes simplex viruses (HSV-1 and HSV-2): These viruses can remain latent in nerve ganglia and reactivate to cause oral or genital herpes.
- Varicella-zoster virus (VZV): This virus causes chickenpox and can later reactivate as shingles.
- Cytomegalovirus (CMV): This virus can remain latent in the body for years and reactivate in individuals with weakened immune systems.
Diagnosing Endogenous Infections
Diagnosing endogenous infections often presents challenges because the causative agent is already present in the body. Diagnosis typically involves:
- Clinical presentation: Symptoms can be variable depending on the causative agent and the site of infection.
- Microbial culture: Identifying the specific microbe through culture from infected tissues or fluids is crucial.
- Molecular diagnostic techniques: PCR and other molecular methods can detect the genetic material of the causative agent, even in low numbers.
- Imaging techniques: X-rays, CT scans, and MRI can help visualize the extent of the infection.
Treatment and Prevention of Endogenous Infections
Treatment for endogenous infections depends on the causative agent, the site of infection, and the severity of the illness. Options include:
- Antibiotics: For bacterial infections, appropriate antibiotics are essential.
- Antifungal medications: For fungal infections, specific antifungals are used.
- Antiviral medications: For viral infections, antiviral drugs may be effective.
- Supportive care: This includes measures to maintain fluid balance, manage pain, and provide respiratory support.
Preventing endogenous infections involves strategies to:
- Strengthen the immune system: A strong immune system is crucial in preventing opportunistic infections. This can be achieved through a healthy lifestyle, including proper nutrition, adequate rest, and stress management.
- Careful antibiotic use: Antibiotics should be used judiciously to prevent disruption of the normal microbiota.
- Hygiene practices: Good hygiene practices, such as proper handwashing, can help prevent the spread of microbes.
- Vaccination: Vaccination against certain pathogens can prevent serious infections.
- Managing underlying conditions: Effective management of underlying diseases can reduce the risk of opportunistic infections.
Conclusion: The Complex Interplay of Host and Microbe
Endogenous infectious agents highlight the complex interplay between the host and its resident microbiota. While the majority of these microbes are beneficial, they can become pathogenic under specific circumstances. Understanding the factors that contribute to this transition is vital for developing effective strategies for diagnosis, treatment, and prevention. Further research into the dynamics of the microbiome and its interaction with the immune system is crucial for improving our ability to combat endogenous infections and maintain a healthy balance within the human body. This includes exploring the potential of novel therapeutic approaches that target specific microbial communities or modulate the immune response to prevent opportunistic infections. The future of battling endogenous infections lies in a holistic approach that integrates our understanding of the human microbiome with advancements in diagnostic and therapeutic technologies. By carefully considering the intricate relationship between host and microbe, we can move toward more effective strategies for promoting health and preventing disease.
Latest Posts
Latest Posts
-
All New Jeep Wagoneer S Launch Quizlet
Mar 23, 2025
-
Its Okay To Take Isotretinoin When Quizlet
Mar 23, 2025
-
What Did The Declaration Of Independence Do Quizlet
Mar 23, 2025
-
What Is The Definition Of A Foreign Corporation Quizlet
Mar 23, 2025
-
Which Condition Is Associated With Acalculous Cholecystitis Quizlet
Mar 23, 2025
Related Post
Thank you for visiting our website which covers about Endogenous Infectious Agents Arise From Microbes That Are . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
