Explain The Differences In The Cognitive Factors Of Somatoform Disorders.
Breaking News Today
Mar 22, 2025 · 5 min read
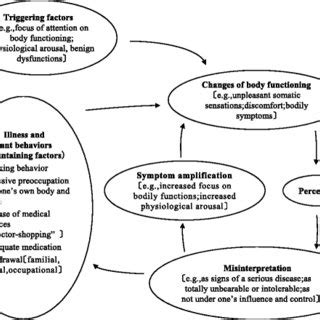
Table of Contents
Decoding the Cognitive Landscape of Somatoform Disorders: A Deep Dive into Differential Factors
Somatoform disorders, a complex tapestry of physical symptoms without identifiable medical causes, are characterized by a significant interplay of cognitive, emotional, and behavioral factors. While the diagnostic criteria may appear similar across various somatoform disorders, a closer examination reveals nuanced differences in the underlying cognitive processes. Understanding these distinctions is crucial for effective diagnosis, treatment, and ultimately, improved patient outcomes. This article delves deep into the cognitive factors underpinning different somatoform disorders, highlighting their unique characteristics and implications.
The Cognitive Core: Shared and Distinct Features
Before exploring individual disorders, it's important to establish a common ground. Many somatoform disorders share some core cognitive features:
1. Heightened Bodily Awareness and Attention:
Individuals with somatoform disorders often exhibit increased attention to bodily sensations. What might be a fleeting discomfort for others becomes a significant source of worry and distress. This heightened awareness is not necessarily pathological; everyone experiences bodily sensations, but in somatoform disorders, the interpretation and reaction to these sensations are significantly amplified.
2. Catastrophizing and Misinterpretation of Symptoms:
A key cognitive distortion is catastrophizing. Minor physical sensations are magnified, interpreted as serious illnesses, and often lead to significant anxiety and fear. The individual may engage in illness-related searching, constantly seeking reassurance from doctors and online sources, further fueling anxiety and reinforcing the belief that something is seriously wrong.
3. Cognitive Distortions and Negative Thoughts:
Negative thinking patterns, such as all-or-nothing thinking, overgeneralization, and personalization, frequently contribute to the maintenance of somatoform symptoms. These distortions fuel anxiety and maintain the focus on physical symptoms. For example, a small headache might be interpreted as an impending brain tumor ("This headache means I have a brain tumor and I'm going to die").
Differential Cognitive Profiles: Exploring Individual Disorders
While the aforementioned cognitive features are common across somatoform disorders, subtle yet crucial differences exist depending on the specific diagnosis:
Somatic Symptom Disorder (SSD):
SSD is characterized by persistent somatic symptoms combined with excessive thoughts, feelings, or behaviors related to these symptoms. The cognitive profile often involves:
- Persistent fear of illness: Individuals with SSD are preoccupied with the fear of having a serious medical condition, even in the absence of specific symptoms. This fear is a central driver of their distress and seeking of medical attention.
- Health anxiety: A chronic state of worry and anxiety about one's health, characterized by frequent self-examination, monitoring bodily sensations, and seeking reassurance.
- Attentional bias towards bodily sensations: A strong tendency to focus on and interpret negatively any physical sensations, even those considered normal.
- Difficulty disengaging from somatic concerns: Individuals struggle to shift their attention away from their physical symptoms, despite reassurances from medical professionals.
Illness Anxiety Disorder (IAD) (formerly Hypochondriasis):
IAD involves a preoccupation with the fear of having or acquiring a serious illness, but without significant somatic symptoms. The key cognitive difference here lies in the absence of prominent physical symptoms. Instead, the distress stems primarily from the fear of illness itself. Cognitive features specific to IAD include:
- High levels of health anxiety: The anxiety is intensely focused on the possibility of illness, driving excessive health-related behaviors like internet searching, self-examination, and seeking reassurance from healthcare providers.
- Interpretative bias: A tendency to interpret ambiguous physical sensations as signs of serious illness. This interpretation is often resistant to reassurance.
- Safety behaviors: Individuals may engage in safety behaviors, such as repeated doctor visits or avoidance of activities perceived as risky, which, paradoxically, reinforce their anxieties.
Conversion Disorder (Functional Neurological Symptom Disorder):
Conversion disorder presents with neurological symptoms, such as paralysis, blindness, or numbness, without a neurological explanation. Cognitive factors play a less dominant role compared to SSD or IAD, but still contribute significantly:
- Emotional distress and psychological conflict: Often, conversion symptoms emerge after significant stress or trauma. The symptoms can be understood as a way of expressing or managing the overwhelming emotions.
- Limited awareness of the psychological connection: Individuals may not consciously connect their symptoms to their psychological distress. This isn't necessarily a lack of insight, but rather a dissociation or lack of awareness of how their emotional state might manifest physically.
- Cognitive avoidance of distress: The symptoms might be a subconscious avoidance strategy, indirectly preventing the individual from confronting the underlying emotional pain.
Factitious Disorder:
Factitious disorder, involves the intentional falsification or induction of physical or psychological symptoms. The cognitive features are distinct and often revolve around:
- Need for attention and sympathy: A profound need to be perceived as sick, which drives the deliberate production of symptoms.
- Intense preoccupation with the medical system: The individual may develop a deep dependence on the medical setting, deriving a sense of identity and belonging from their illness narrative.
- Secondary gain: While not always conscious, there might be an unconscious desire for attention, sympathy, or avoidance of responsibilities that reinforces the behavior. This is distinctly different from malingering, where the motivation is external gain (e.g., financial compensation).
Therapeutic Implications of Cognitive Understanding
Recognizing these distinct cognitive profiles is essential for tailoring effective treatment approaches. Cognitive behavioral therapy (CBT) is a cornerstone treatment for many somatoform disorders. CBT targets the specific cognitive distortions and maladaptive behaviors associated with each disorder. For example:
- In SSD and IAD: CBT focuses on challenging catastrophic thinking, reducing health anxiety, developing coping mechanisms for managing bodily sensations, and promoting a more balanced perspective on health.
- In Conversion Disorder: CBT may involve exploring the underlying emotional conflicts, teaching relaxation techniques, and promoting self-awareness of the connection between emotions and symptoms.
- In Factitious Disorder: Treatment is complex and often requires a multidisciplinary approach involving psychotherapy, psychiatry, and potentially other specialists.
Conclusion: The Interwoven Nature of Cognitive Factors
The cognitive factors in somatoform disorders are not isolated entities; they are intricately interwoven with emotional and behavioral components. Understanding these interactions is key to providing comprehensive and effective care. The differences outlined above highlight the need for a nuanced approach to assessment and treatment, tailored to the specific cognitive profile and challenges faced by each individual. Further research into the neural underpinnings of these cognitive processes will further enhance our understanding and ultimately lead to more effective interventions for those affected by these complex disorders. The future lies in a more holistic approach, integrating the cognitive, emotional, and social dimensions of these conditions to improve the lives of those who experience them.
Latest Posts
Latest Posts
-
Accounting Is The Information System That Quizlet
Mar 23, 2025
-
What Happened At The Constitutional Convention Quizlet
Mar 23, 2025
-
The Bioavailability Of Vitamins In Food Quizlet
Mar 23, 2025
-
Ulcerative Colitis Is Commonly Associated With Quizlet
Mar 23, 2025
-
How Was The Cuban Missile Crisis Resolved Quizlet
Mar 23, 2025
Related Post
Thank you for visiting our website which covers about Explain The Differences In The Cognitive Factors Of Somatoform Disorders. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
