Ulcerative Colitis Is Commonly Associated With Quizlet
Breaking News Today
Mar 23, 2025 · 7 min read
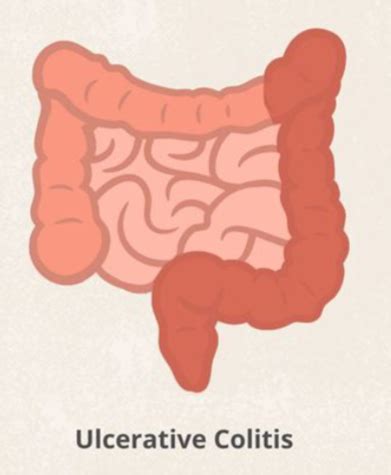
Table of Contents
Ulcerative Colitis: Commonly Associated Factors and Conditions
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the large intestine (colon) and rectum. Characterized by inflammation and ulceration of the inner lining of the colon, UC can manifest in a range of symptoms, from mild discomfort to severe complications. While the exact cause of UC remains unknown, extensive research points to a complex interplay of genetic predisposition, environmental factors, and immune system dysfunction. This article delves into the various factors commonly associated with ulcerative colitis, providing a comprehensive overview of its intricate nature.
Genetic Predisposition: The Family History Factor
A significant risk factor for developing ulcerative colitis is a family history of IBD. Individuals with a first-degree relative (parent, sibling, or child) who has UC or Crohn's disease (another type of IBD) have a substantially increased risk of developing the condition themselves. This genetic susceptibility isn't deterministic; it simply increases the probability. While specific genes haven't been definitively pinpointed as the cause, numerous gene variations have been identified that contribute to the increased risk. These genetic variations often influence immune response regulation and inflammation pathways within the gut. Understanding family history is crucial in assessing individual risk and guiding preventative measures and early detection strategies.
HLA Genes and IBD Risk: A Deeper Dive
Human leukocyte antigen (HLA) genes play a crucial role in the immune system's ability to distinguish between self and non-self. Certain HLA alleles (variants) have been strongly associated with increased risk for UC. These alleles influence the presentation of antigens (foreign substances) to immune cells, potentially triggering an inappropriate immune response against the gut lining, leading to inflammation characteristic of UC. Research continues to unravel the complex interactions between specific HLA alleles and the development of ulcerative colitis.
Environmental Triggers: Exacerbating the Risk
While genetics play a significant role, environmental factors also contribute to the development and progression of ulcerative colitis. These factors aren't necessarily the primary cause, but rather act as triggers or exacerbators in genetically susceptible individuals. The intricate interplay between genetics and environment is crucial to understand the disease's complexity.
Diet and Nutrition: The Gut Microbiome Connection
The role of diet in UC is multifaceted and actively researched. While there's no single "UC diet," certain dietary patterns and components may influence gut health and inflammation. A diet rich in fiber, fruits, and vegetables, alongside a balanced intake of macronutrients, is generally recommended. Conversely, excessive consumption of processed foods, red meat, and saturated fats may exacerbate inflammation. The gut microbiome, the complex ecosystem of bacteria and other microorganisms residing in the gut, is also deeply intertwined with UC. Imbalances in the gut microbiome (dysbiosis) are commonly observed in individuals with UC, potentially contributing to chronic inflammation.
Infections: A Potential Culprit
Certain infections, particularly those targeting the gut, have been implicated as potential triggers or exacerbators of ulcerative colitis. While not definitively causal, these infections might initiate or worsen the inflammatory process in already susceptible individuals. The precise mechanisms by which infections contribute to UC remain under investigation, but theories suggest that an altered immune response following infection may contribute to the development of the disease.
Smoking: A Significant Risk Factor
Smoking is a significant risk factor for ulcerative colitis, and it appears to worsen the disease’s course and prognosis. Studies have consistently demonstrated a link between smoking and a higher risk of developing UC, as well as an increased likelihood of more severe disease, including the need for surgery. The exact mechanisms by which smoking affects UC are not fully understood, but it's likely related to its effects on the immune system and gut microbiome. Quitting smoking is strongly advised for individuals with UC or at increased risk.
Immune System Dysfunction: The Central Player
At the heart of ulcerative colitis lies an aberrant immune response. The immune system, instead of tolerating the gut lining, mistakenly attacks it, leading to inflammation and ulceration. This inappropriate immune response involves various immune cells, including T cells, B cells, and macrophages.
Cytokines and Inflammatory Mediators: The Molecular Mechanisms
A hallmark of UC is the increased production of pro-inflammatory cytokines, signaling molecules that amplify inflammation. These cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-6, and IL-1β, are implicated in the damage and destruction of the colonic mucosa. Understanding the specific roles of these cytokines and other inflammatory mediators is crucial for developing targeted therapies.
Genetic Variations Affecting Immune Response: The Underlying Mechanisms
Genetic variations influencing immune response regulation are central to understanding the susceptibility to ulcerative colitis. Variations in genes affecting immune cell development, activation, and function can contribute to an inappropriate immune response against the gut lining. This dysregulated immune response is a key driver of the chronic inflammation characteristic of the disease.
Commonly Associated Conditions: The Comorbidities
Ulcerative colitis is frequently associated with several other conditions, often referred to as comorbidities. These conditions may share similar underlying pathophysiological mechanisms or result from the impact of UC itself.
Extraintestinal Manifestations: Beyond the Gut
UC isn't confined to the gastrointestinal tract. Many individuals with UC experience extraintestinal manifestations—symptoms affecting other parts of the body. These can include:
- Skin manifestations: Pyoderma gangrenosum (a severe skin ulceration), erythema nodosum (painful nodules under the skin), and psoriasis are common skin conditions associated with UC.
- Joint problems: Arthritis (inflammation of joints) is a frequent comorbidity, often involving peripheral joints such as knees and ankles. Sacroiliitis (inflammation of the sacroiliac joints) can also occur.
- Eye problems: Uveitis (inflammation of the eye) and episcleritis (inflammation of the white of the eye) are eye problems linked to UC.
- Liver disease: Primary sclerosing cholangitis (PSC), a chronic liver disease, is strongly associated with UC.
- Kidney problems: Kidney stones are more common in individuals with UC.
Mental Health Considerations: The Psychological Impact
Living with a chronic condition like ulcerative colitis can significantly impact mental health. Anxiety, depression, and stress are common comorbidities associated with UC. The chronic nature of the disease, unpredictable symptoms, and the need for ongoing medical management can contribute to psychological distress. Addressing mental health alongside physical health is crucial for comprehensive management of UC.
Nutritional Deficiencies: A Consequence of Inflammation
Chronic inflammation in UC can lead to nutritional deficiencies. Malabsorption of nutrients, due to inflammation and alterations in gut function, can result in deficiencies of vitamins (such as B12, D, and K), iron, and other essential nutrients. Adequate nutrition is crucial for managing UC and preventing complications.
Increased Cancer Risk: A Serious Consideration
Individuals with ulcerative colitis have an increased risk of colorectal cancer. The chronic inflammation associated with UC can damage the lining of the colon, potentially leading to the development of precancerous polyps and eventually cancer. Regular colonoscopies are vital for early detection and prevention of colorectal cancer in individuals with UC.
Diagnosis and Management of Ulcerative Colitis
Accurate diagnosis of ulcerative colitis is crucial for effective management. This typically involves a combination of:
- Medical history and physical examination: A detailed assessment of symptoms, medical history, and family history is the first step.
- Endoscopy: Colonoscopy and sigmoidoscopy allow visualization of the colonic lining, enabling direct assessment of inflammation and ulceration.
- Biopsies: Tissue samples taken during endoscopy are analyzed to confirm the diagnosis and assess the severity of inflammation.
- Imaging studies: Abdominal X-rays, CT scans, and MRIs may be used in specific cases to rule out other conditions or assess complications.
Managing ulcerative colitis focuses on controlling inflammation and relieving symptoms. This often involves a combination of:
- Medications: Various medications are used, including aminosalicylates, corticosteroids, immunomodulators, and biologics, depending on the severity of the disease.
- Lifestyle modifications: Dietary changes, stress management techniques, and smoking cessation are important components of management.
- Surgery: In severe cases, surgery (colectomy) may be necessary to remove the affected portion of the colon.
Conclusion: A Holistic Approach to Ulcerative Colitis
Ulcerative colitis is a complex disease with a wide range of associated factors and conditions. Understanding the interplay of genetic predisposition, environmental triggers, immune system dysfunction, and associated comorbidities is essential for effective diagnosis and management. A holistic approach, encompassing medical interventions, lifestyle modifications, and mental health support, is crucial to improving the quality of life for individuals affected by this chronic inflammatory bowel disease. Ongoing research continues to unravel the intricate mechanisms of UC, leading to the development of new diagnostic tools and therapeutic strategies aimed at improving patient outcomes. Early detection, proactive management, and a collaborative relationship between patient and healthcare provider are fundamental to successfully navigating the challenges of living with ulcerative colitis.
Latest Posts
Latest Posts
-
Compare And Contrast Characteristics Of Healthy Versus Unhealthy Relationships
Mar 25, 2025
-
According To Florida Law What Must Be Aboard A Vessel
Mar 25, 2025
-
Decreasing Term Insurance Is Often Used To
Mar 25, 2025
-
How Do Elephants And Lions Use Carbohydrates
Mar 25, 2025
-
Which Of The Following Is An Example Of Vicarious Punishment
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Ulcerative Colitis Is Commonly Associated With Quizlet . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
